We often form friendships with people who have similar hobbies and interests as we do. However, what happens when chronic illness takes away our ability to take part in those activities? Those friendships often cease to exist because we no longer have ” things in common”. This does not happen just with having a chronic illness – but at times friendships just tend to grow apart. Our hobbies and interests may change over time as well as our life goals – it is just how life goes.

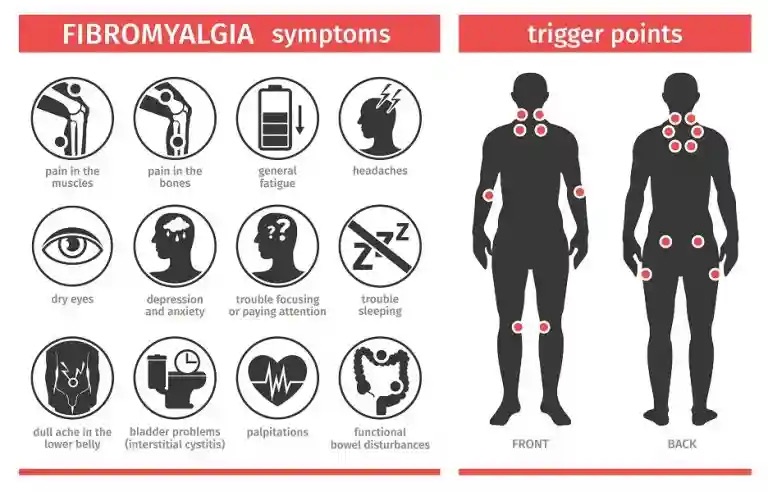
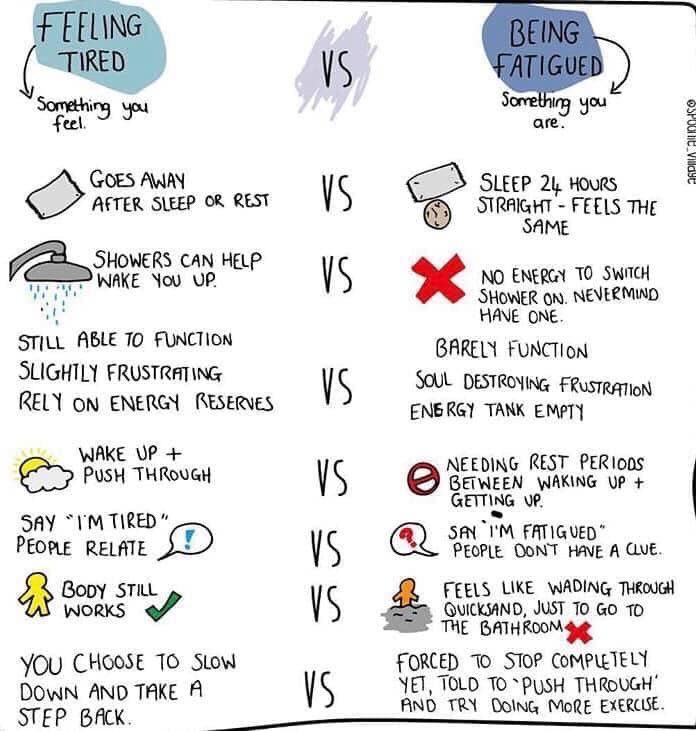
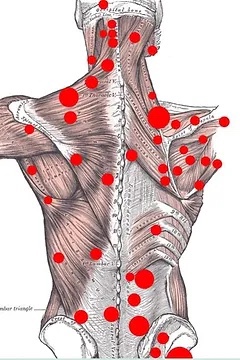
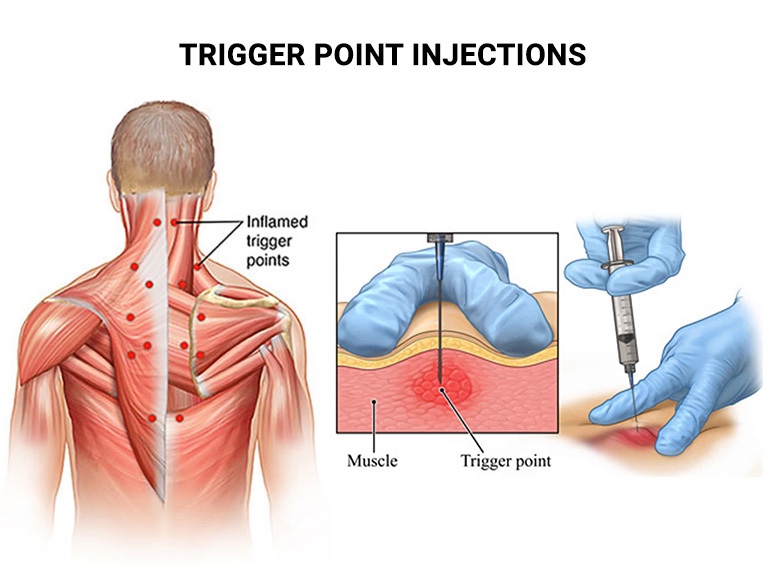
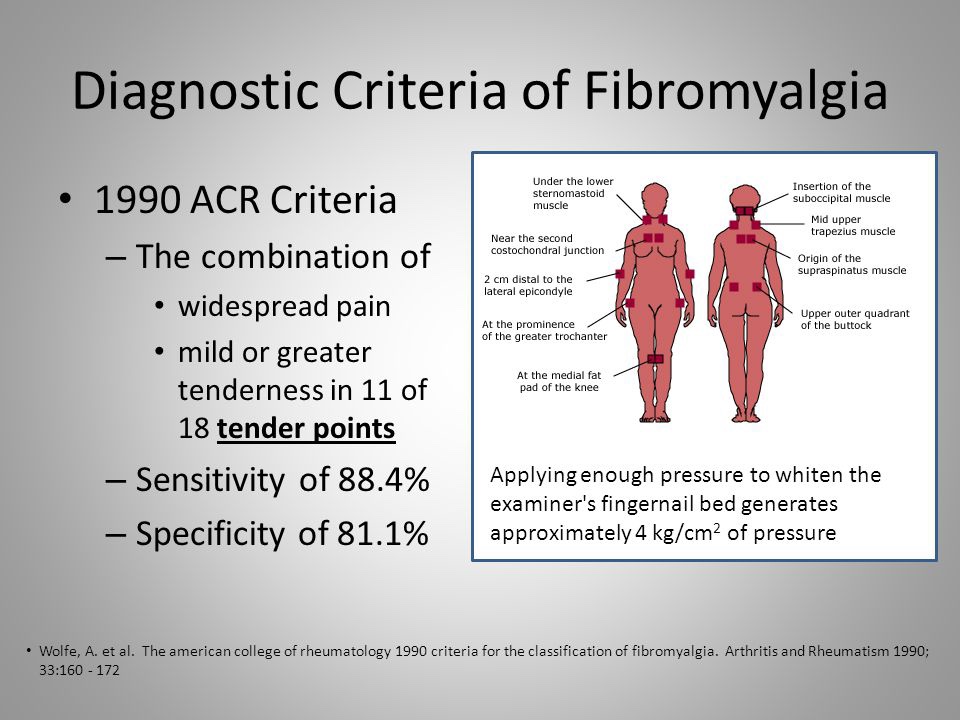
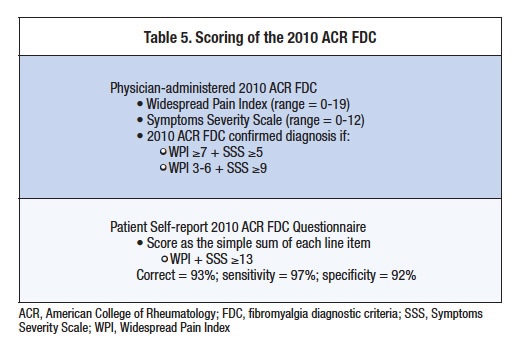
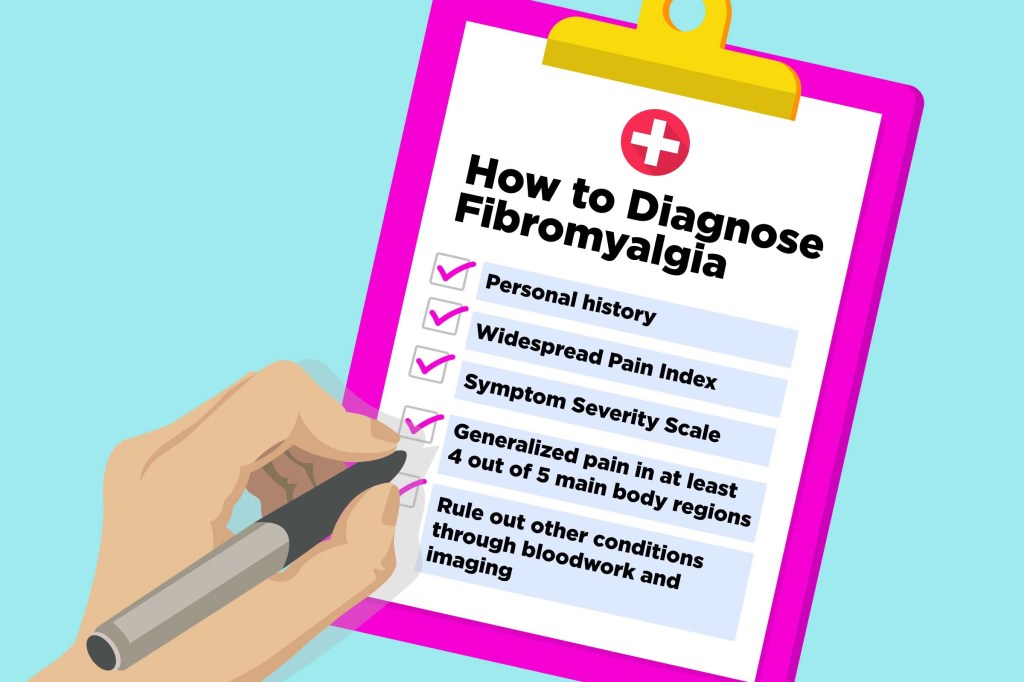
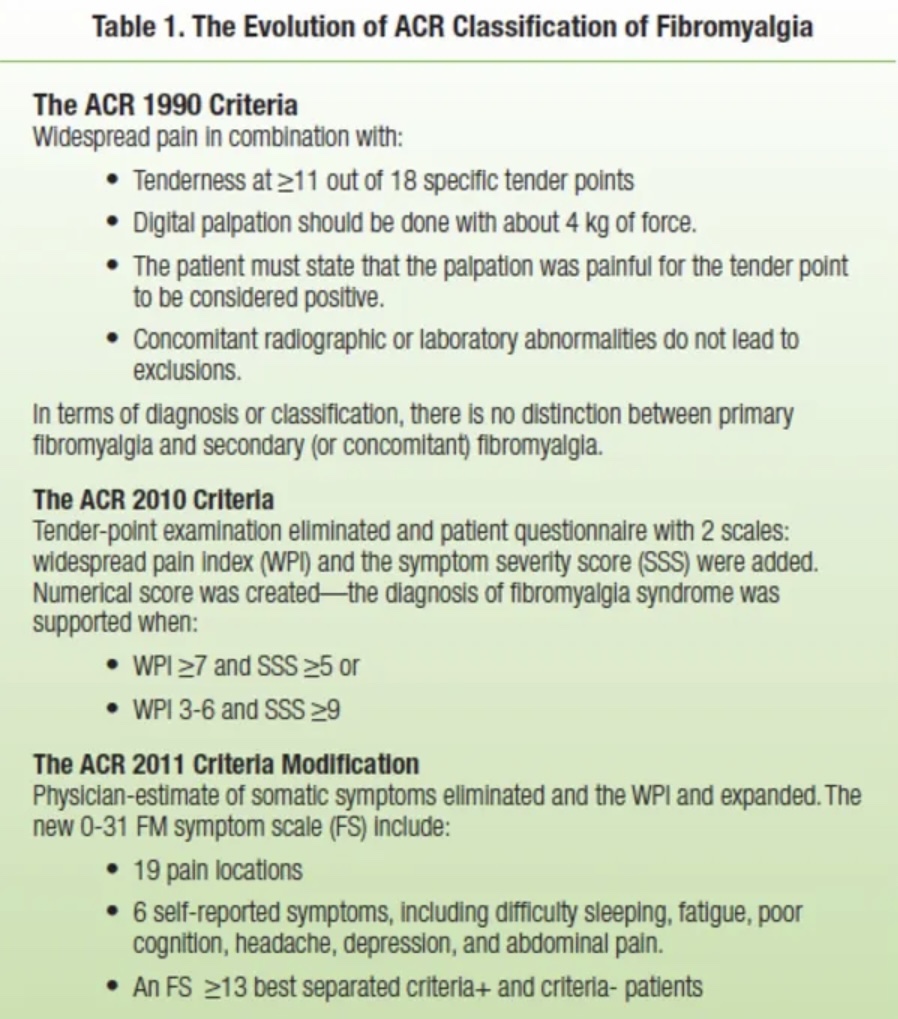
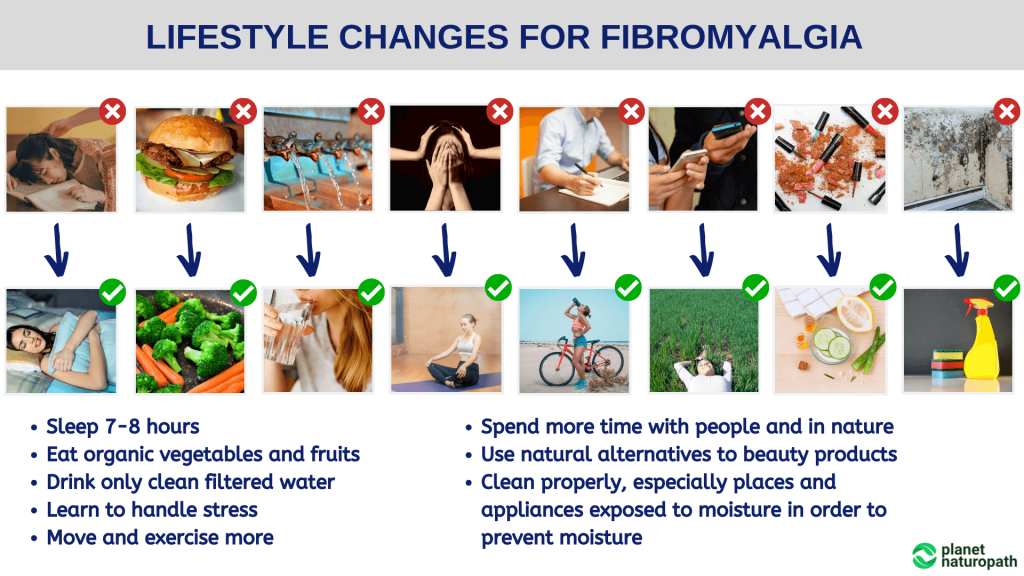
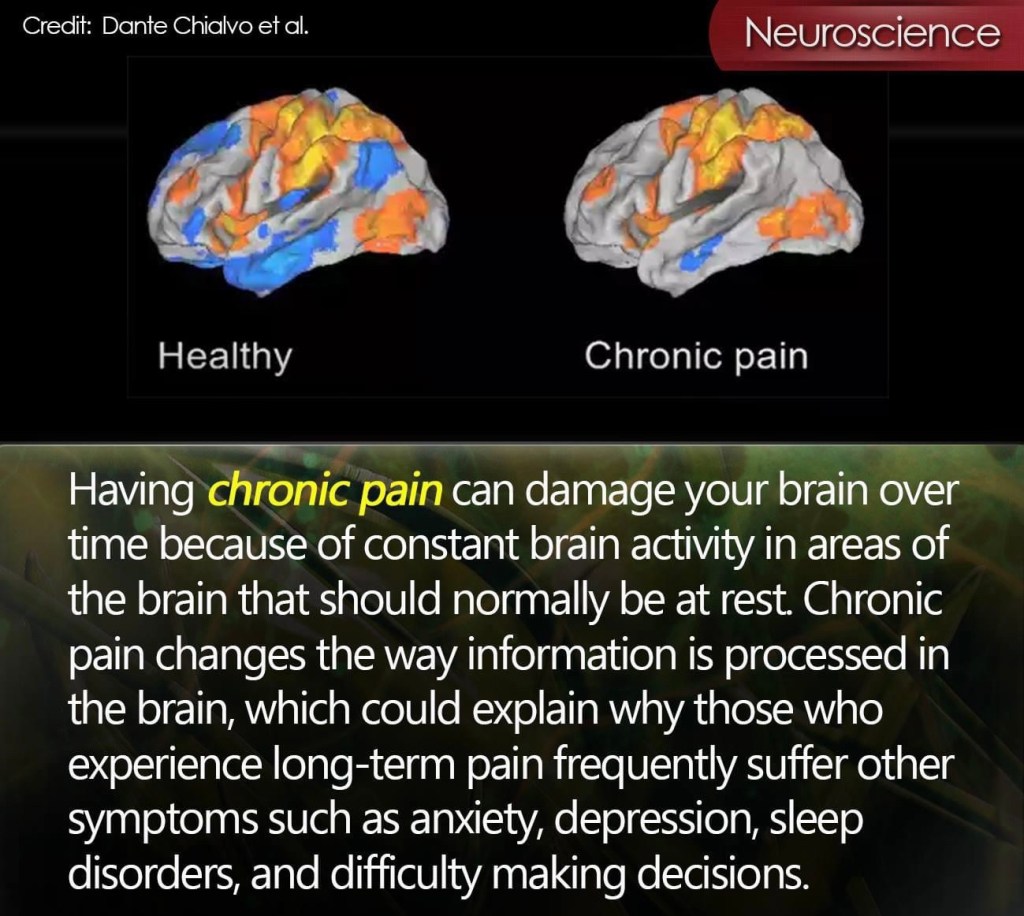
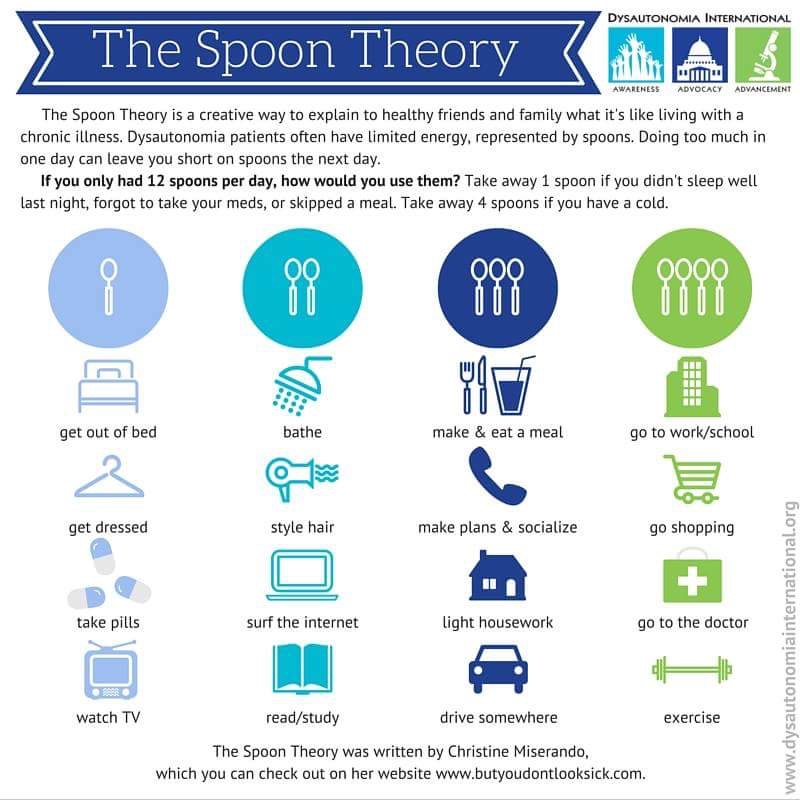
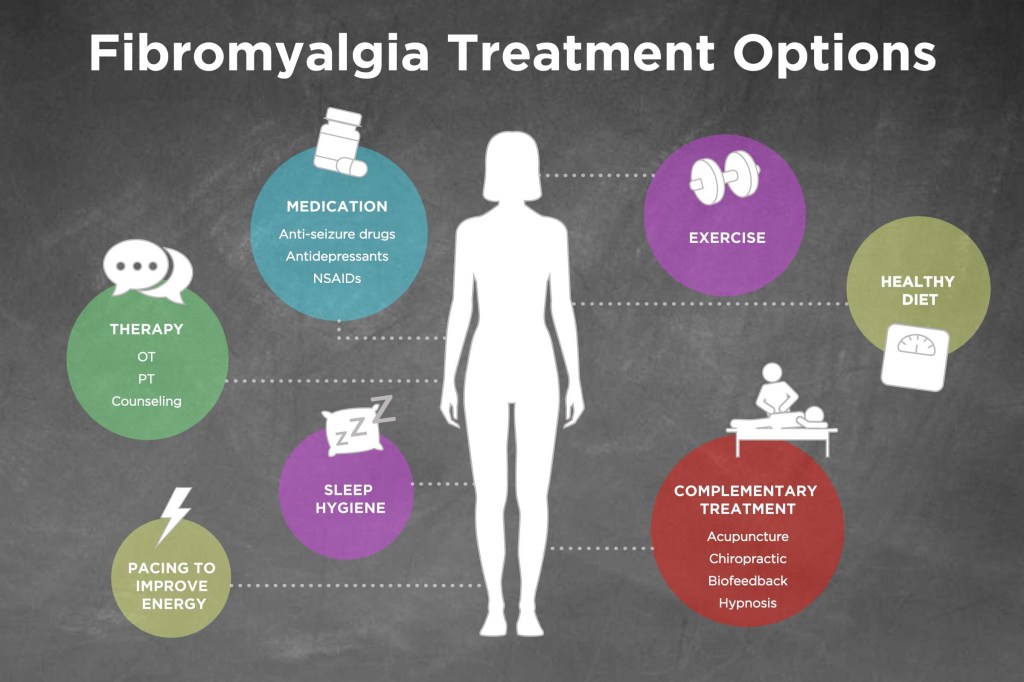
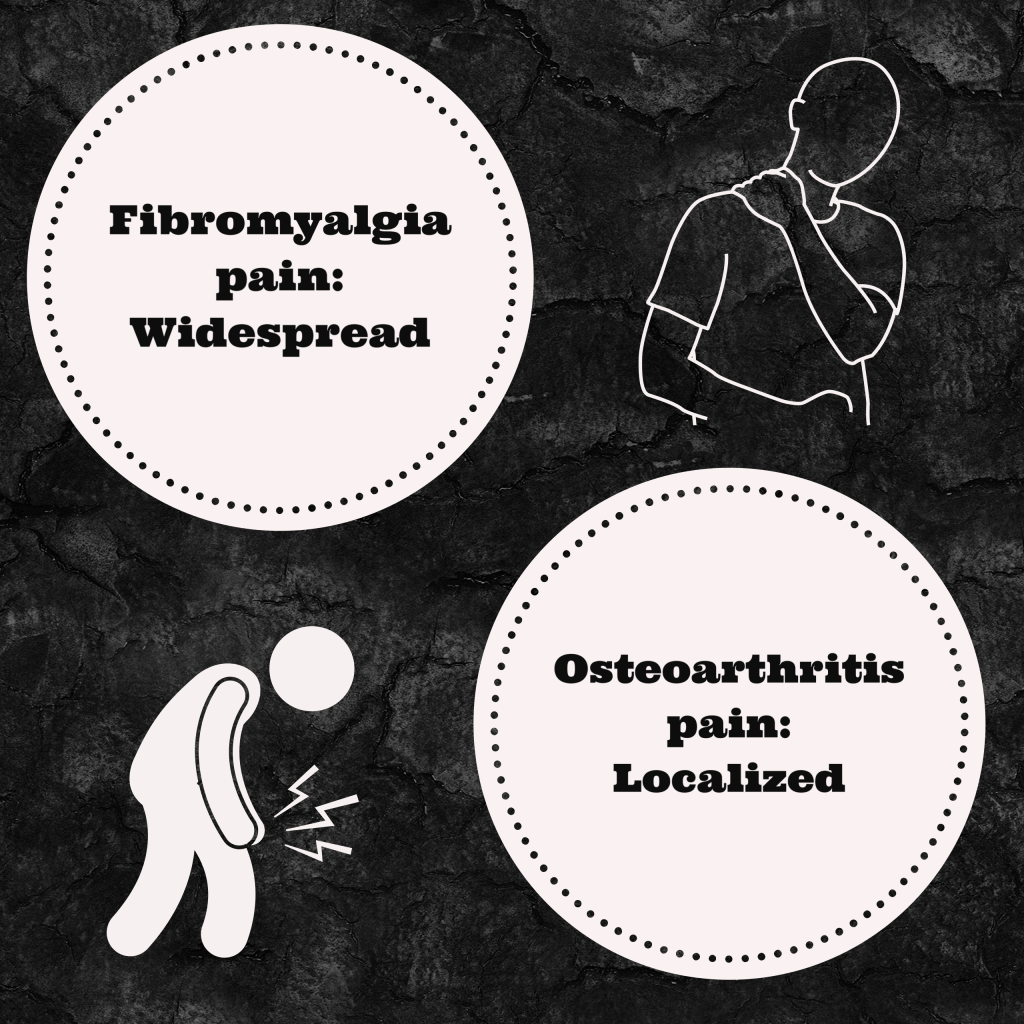
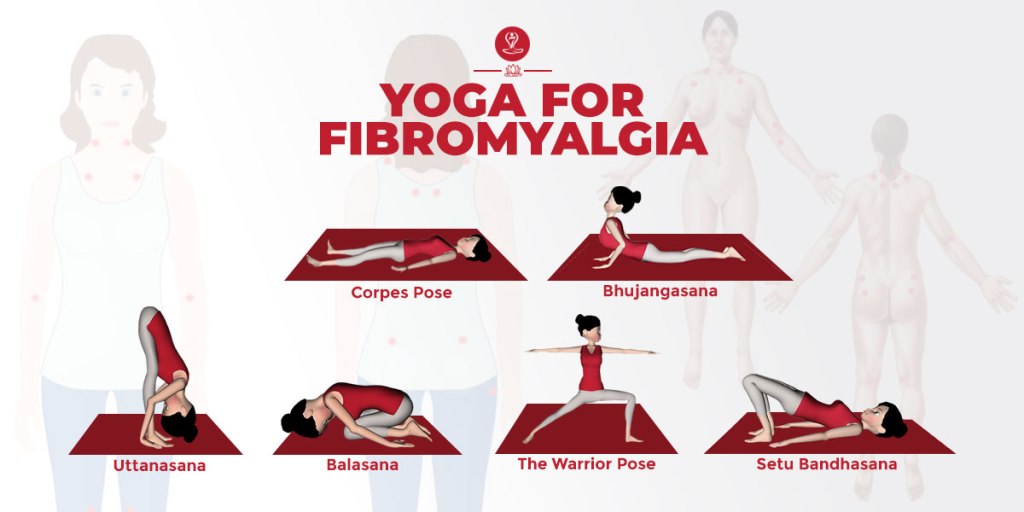
How do we make new friends when we have a chronic illness? I often found it difficult to make new friends as an adult before chronic illness set in- it seems like unless one is into the bar scene it is near impossible. It is even harder when you factor in a chronic illness. I soon realized I was hearing from friends less and less even if I reached out first – messeges often showed read and I received no response. For myself, when I got diagnosed with fibromyalgia in 2019, I started joining online support groups to be able to interact and chat to other people who understood the struggle with chronic pain and every other symptom fibromyalgia seems to throw at us. I found a few people on the group that lived locally and we started going out for lunch or coffee. There was never any hurt feelings if we had to cancel last minute due to not feeling well. I later started fibrofighters – there are quite a few followers who I speak to daily, eventually adding them to my personal Facebook account and consider them to be some of my closest friends. I can always count on them to be there to listen to my struggles even though they are half way around the world. They get it! Strange how people who you have never met can become your main support systems.
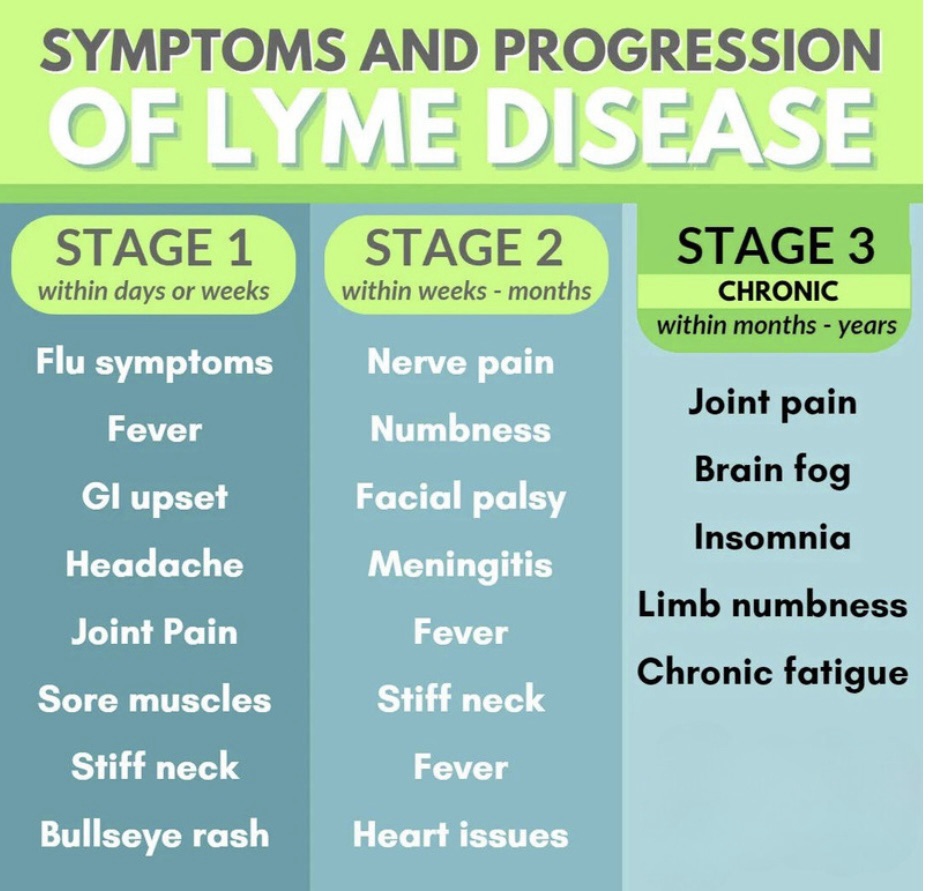
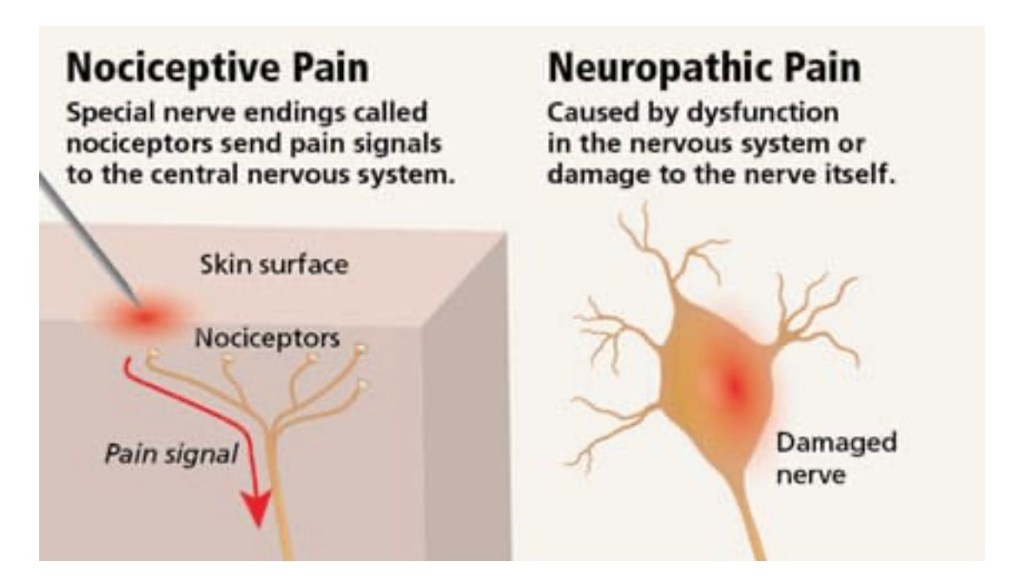
In April 2024, when I received my lyme diagnosis I found myself facing another bout of lost friendships. When I expressed how disappointed I was in “friends” reactions to being diagnosed with lyme disease to the doctor treating me, she looked at me and asked me one simple question , ” Do you really want/need people like that in your life?” Of course my answer was no. Even though it still stung for several weeks, she was right – I don’t need people like that in my life. These “friends” decided to voice their opinions on my treatment routes – it is fine to have an opinion ( we all have opinions), but was it necessary to launch a personal attack and name call?! NO!! You would think my decisions were impacting their lives directly – when they were not. I know their responses were due to lack of knowledge on lyme – however this did not give them the right to treat me in this manner.

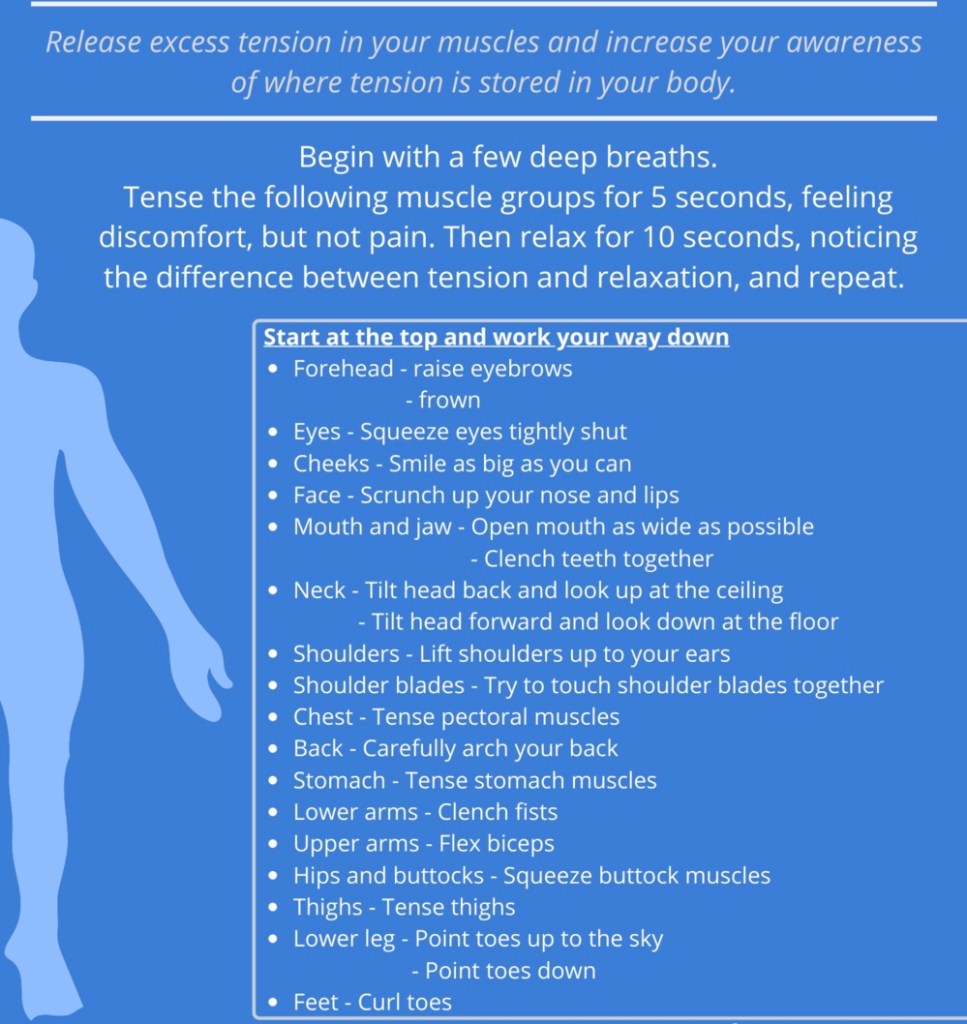
We can’t control how people react and respond, but what we can control is how we react and respond to them. Over the last week I have been listening to Mel Robbins “The Let Them Theory” audiobook. It has been an eye opener for me. I won’t be going into detail about the book itself in my blog as there is just too much information to cover. ” The Let Them Theory” has gone viral and was only published December 24, 2024! I kept seeing her book in every store I went into the last several weeks, so I decided to listen to the audiobook version.
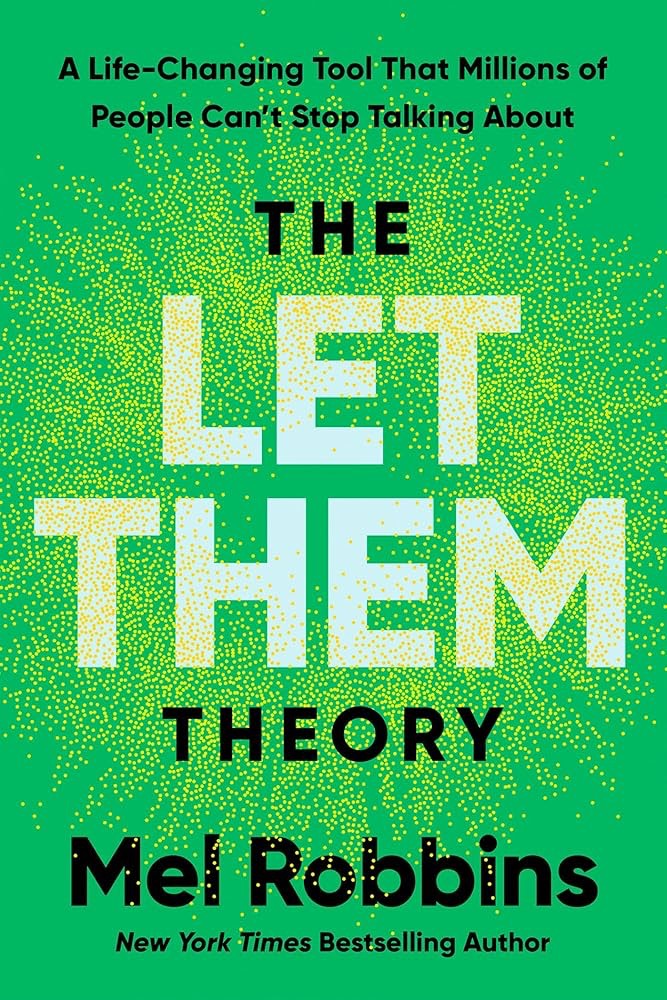
“If they want to leave… let them.
If they choose someone else…let them.
If they don’t support you…let them.
If they don’t invite you…let them.
Stop wasting your energy trying to change or control other people.
Let them show who they really are.
And then you can choose what you do next!”
These seven sentences resonated with me. I felt a sense of peace take over. I realized “friends” opinions and actions reflect who they are, not who I am as a person. The way I respond reflects who I am. I wish I knew about this theory months ago when these situations took place. I would have responded way differently. I think I am going to put this theory to the test. It is going to take time and commitment – but I think it will also better my mental health and over all well being.
LET THEM!