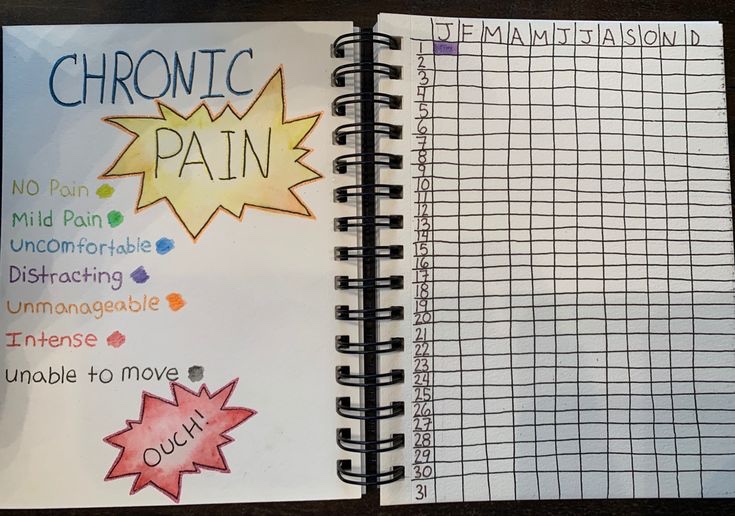
I recently had to attend a doctor’s appointment with a doctor who had ordered a lung function test way back in the fall. At the end of August I got extremely sick with what she thought was pneumonia. After weeks of antibiotics, trips to the emergency room and the cough worsening over time, she decided to order further testing on my lungs.

Fast forward to a few weeks ago…2025
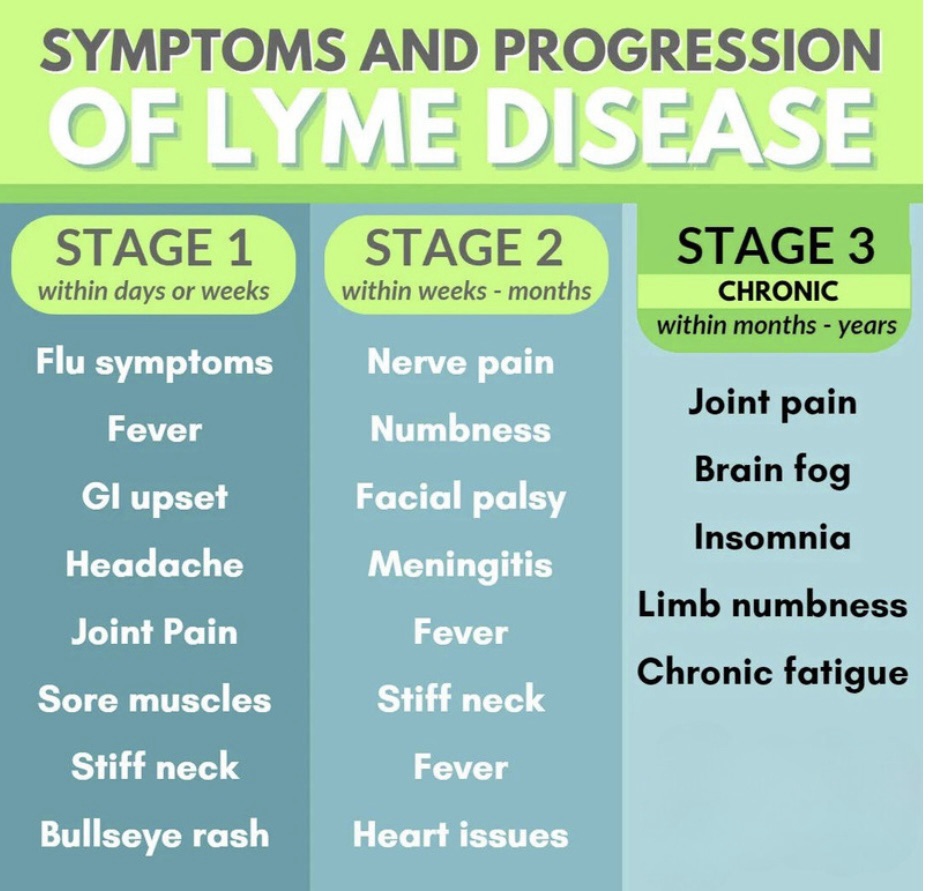
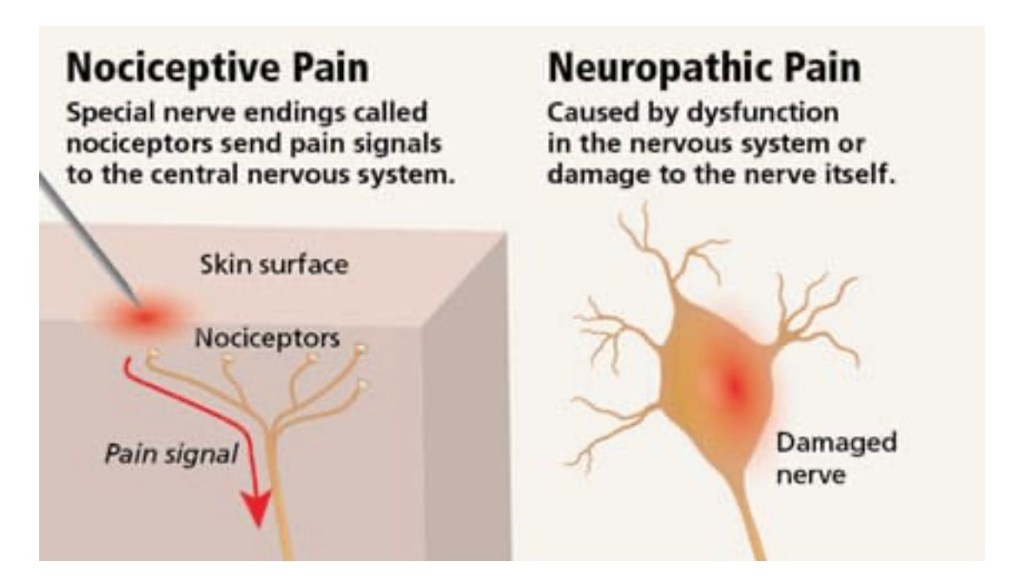
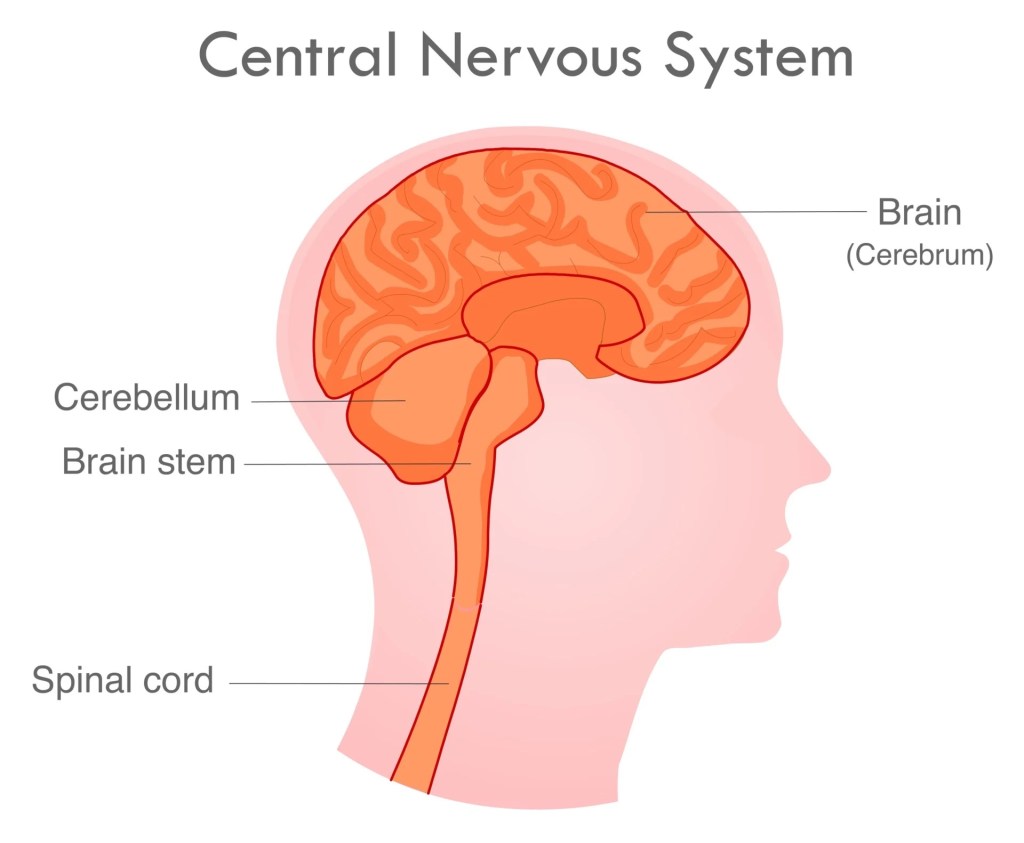
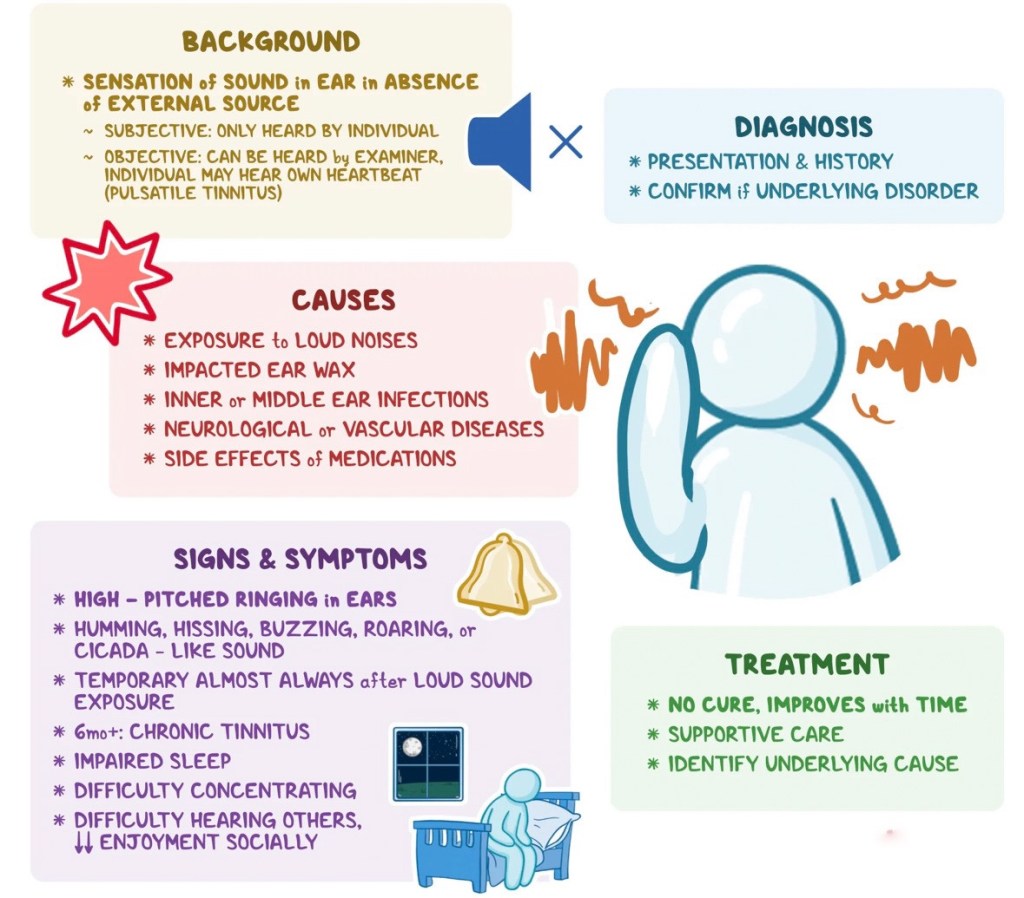
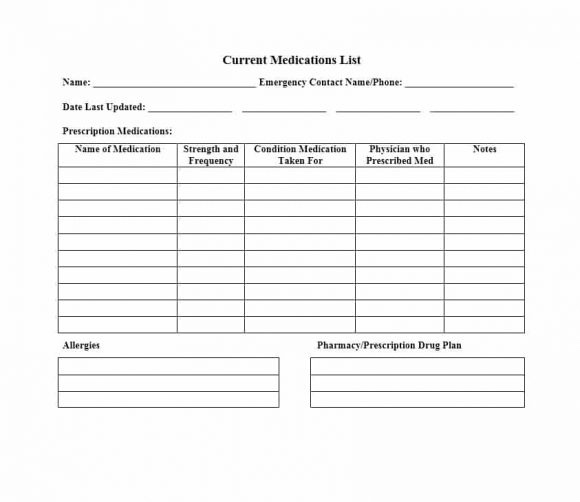
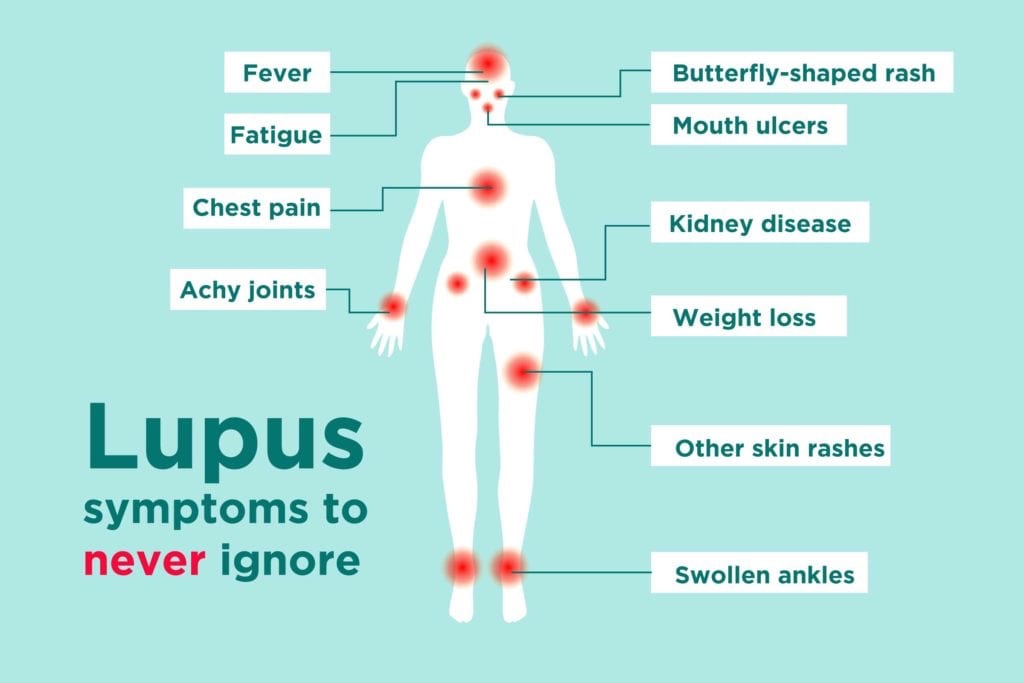
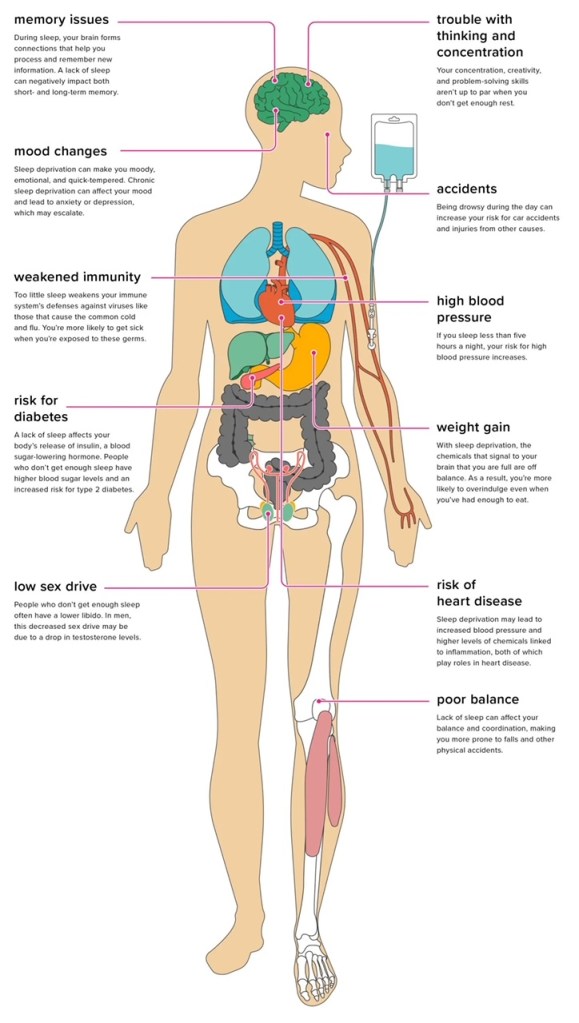
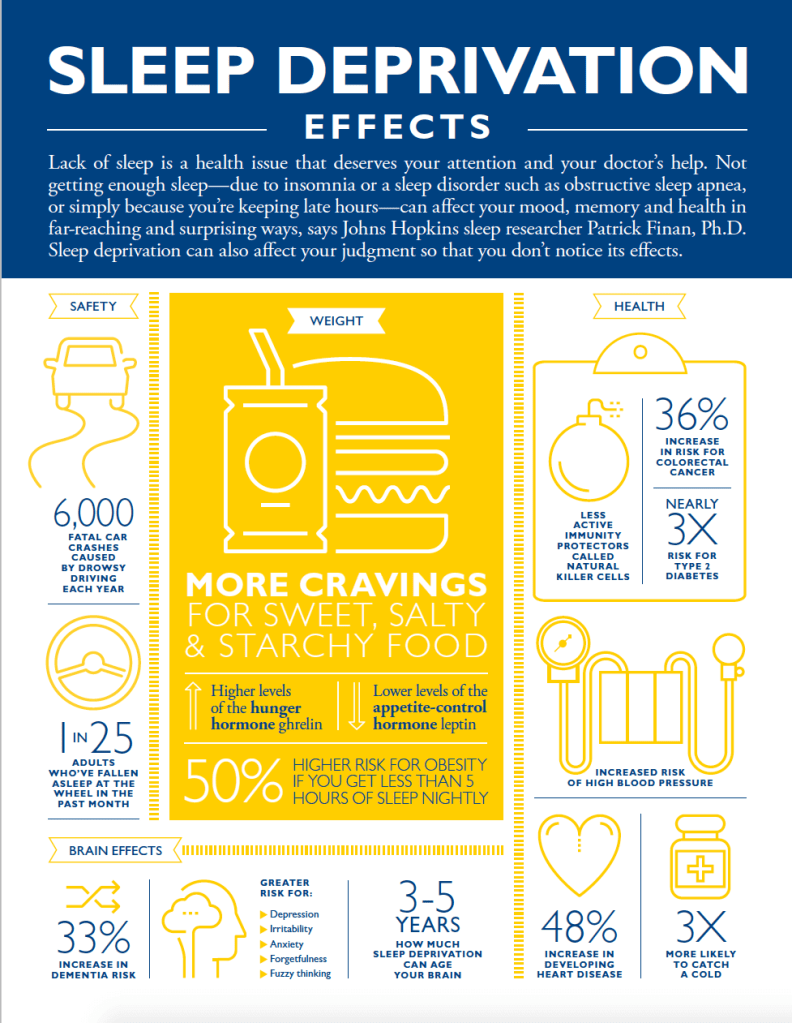
My results were normal. The doctor was left puzzled to why I got a viral infection which worsened by the day for almost two months straight – instead of getting better over time. “The test results don’t make sense. They don’t match how sick you got and for the duration.” I knew it was lyme and bartonella complicating my health struggles – lyme is known for shutting down the immune system from functioning properly and bartonella co infection is known to affect one’s respiratory system. After ten months of not informing my doctor of the lyme diagnosis, I decided to “let it slip”. I decided to bring up lyme due to the fact that I do think it is impacting my lungs in some capacity. You may be wondering why I withheld such important information – most medical doctors do not believe in lyme.

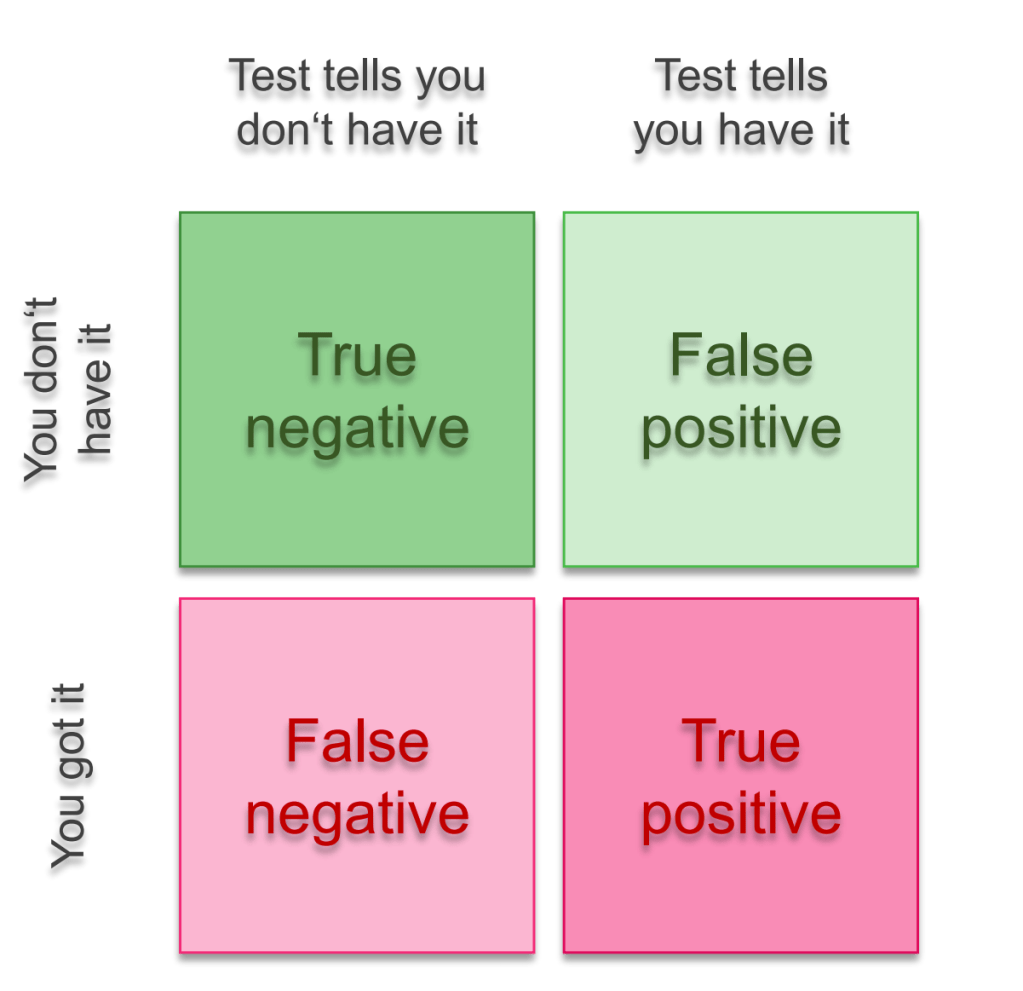
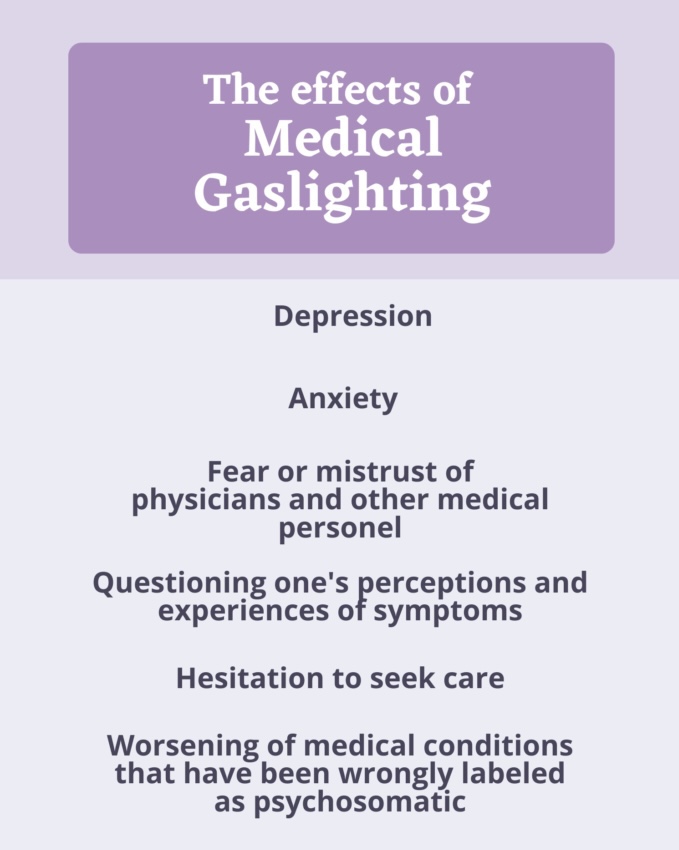
I had prepared myself for her reaction – which was exactly what I expected. I was told the lyme tests are unreliable and most likely I had a false positive. She is right, the two tier lyme tests are unreliable and often produce FALSE NEGATIVES even if one has lyme disease. It is very RARE to have a lyme test produce a false positive. However, the lyme test I had done is more in depth and is even recommended by Canlyme ( Canadian lyme disease foundation). We are also told over and over again that we do not have ticks here or have ticks that carry lyme disease – I totally disagree with this statement.
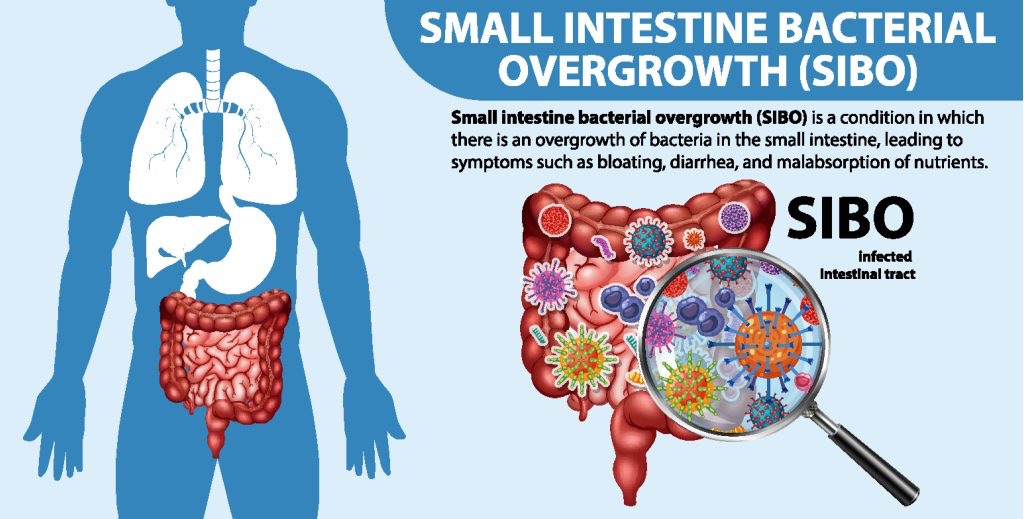
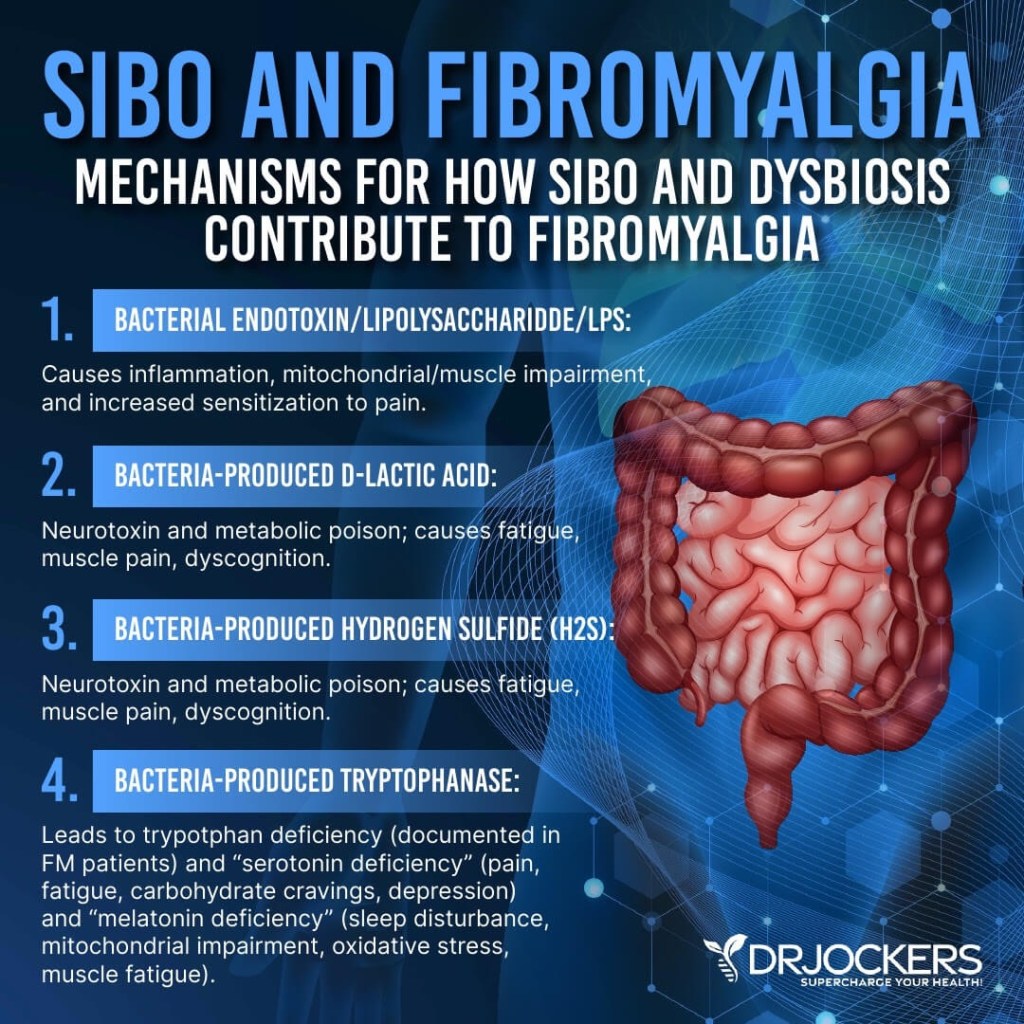
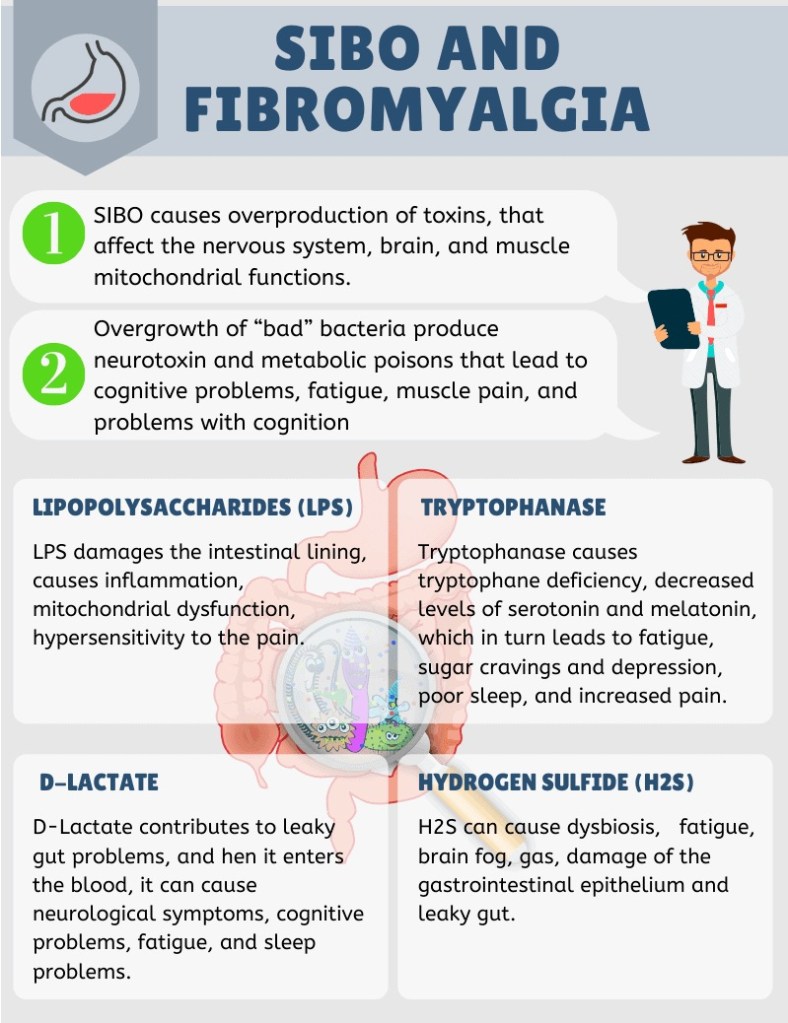
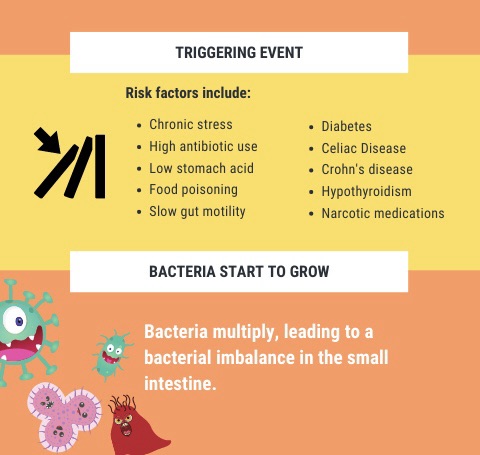
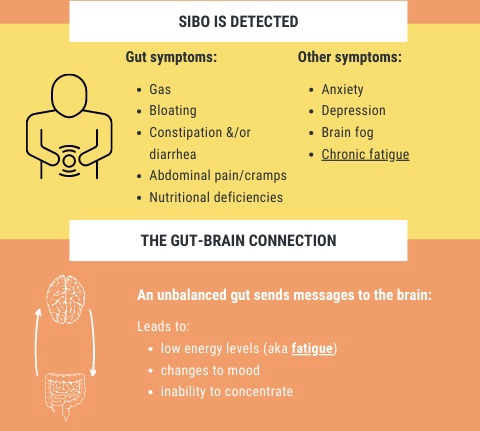
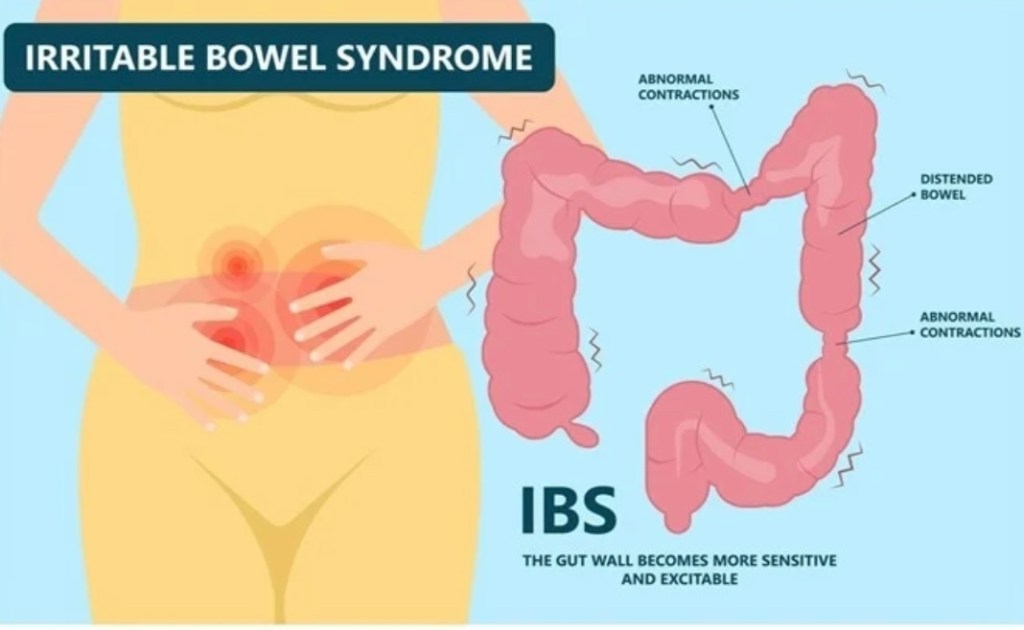
I also mentioned the SIBO gut issues I was being treated for -“SIBO is controversial, we don’t really know if it is a thing!” Say what? If you do a quick google search on SIBO, thousands of medical articles are found. In a matter of a minute, two of my biggest health struggles at the moment were dismissed just like that! I did get referred to a pulmonary specialist – maybe the specialist will be able to to run more in depth testing on my lungs.

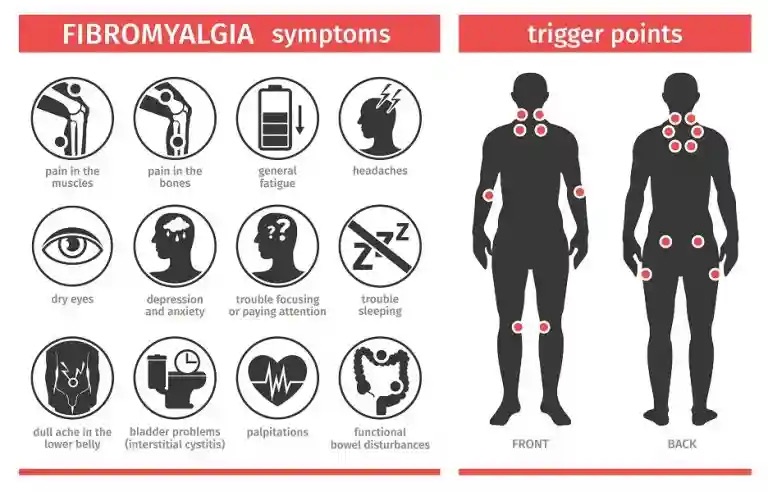
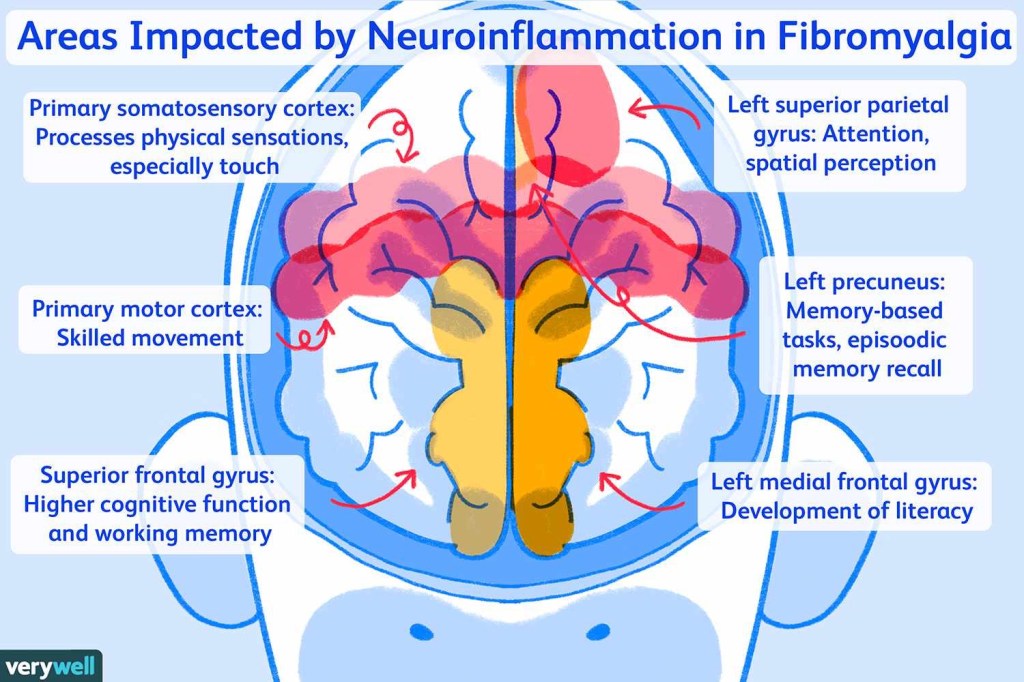
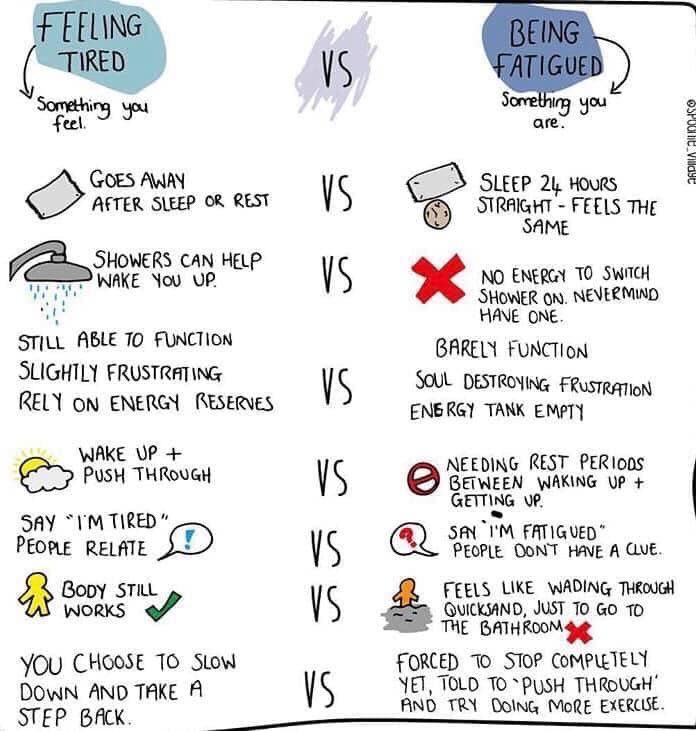
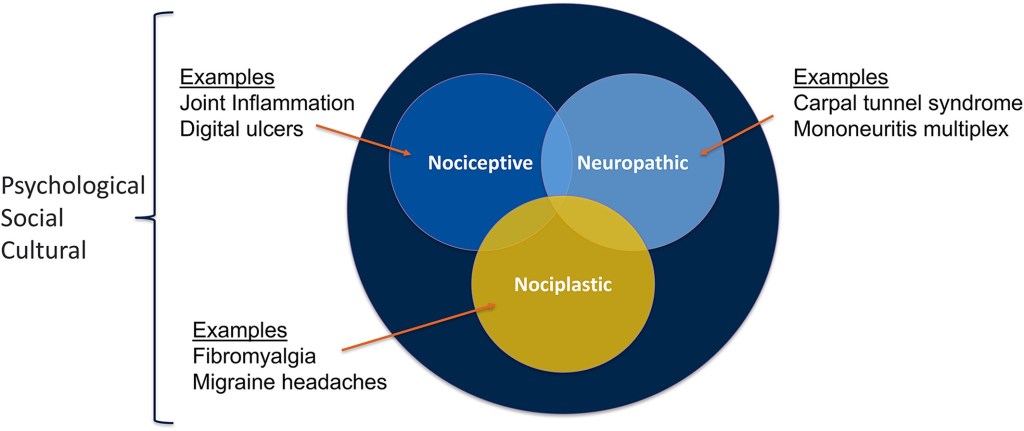
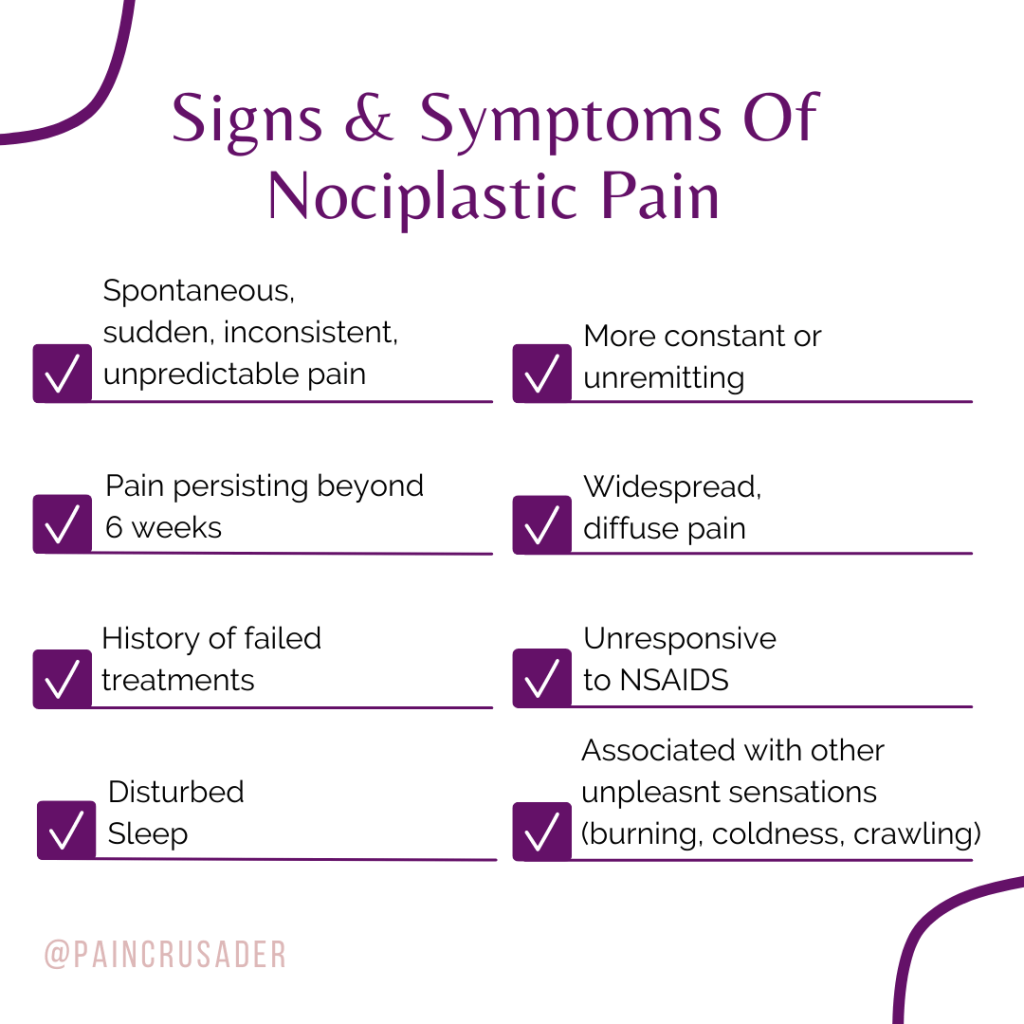
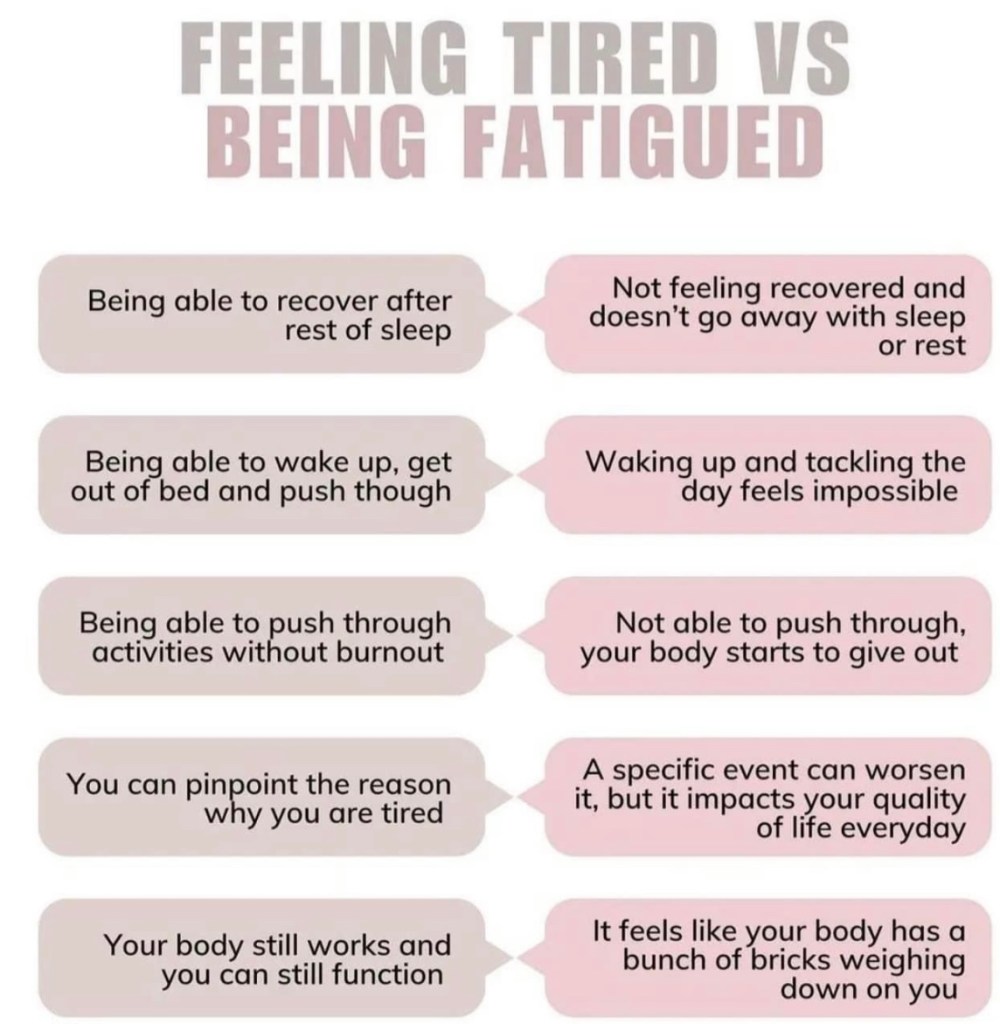
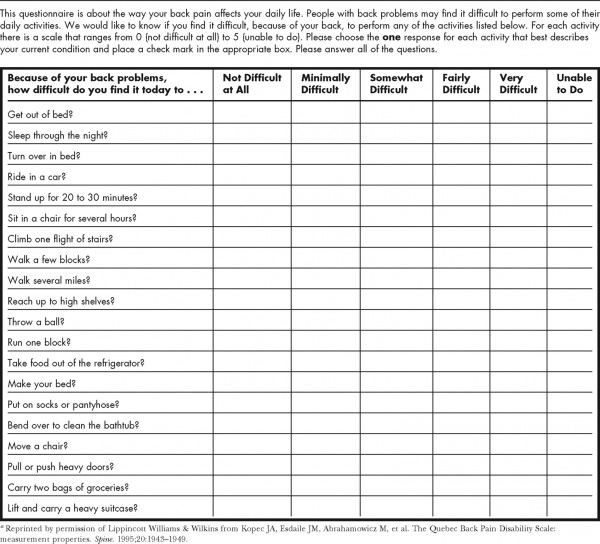
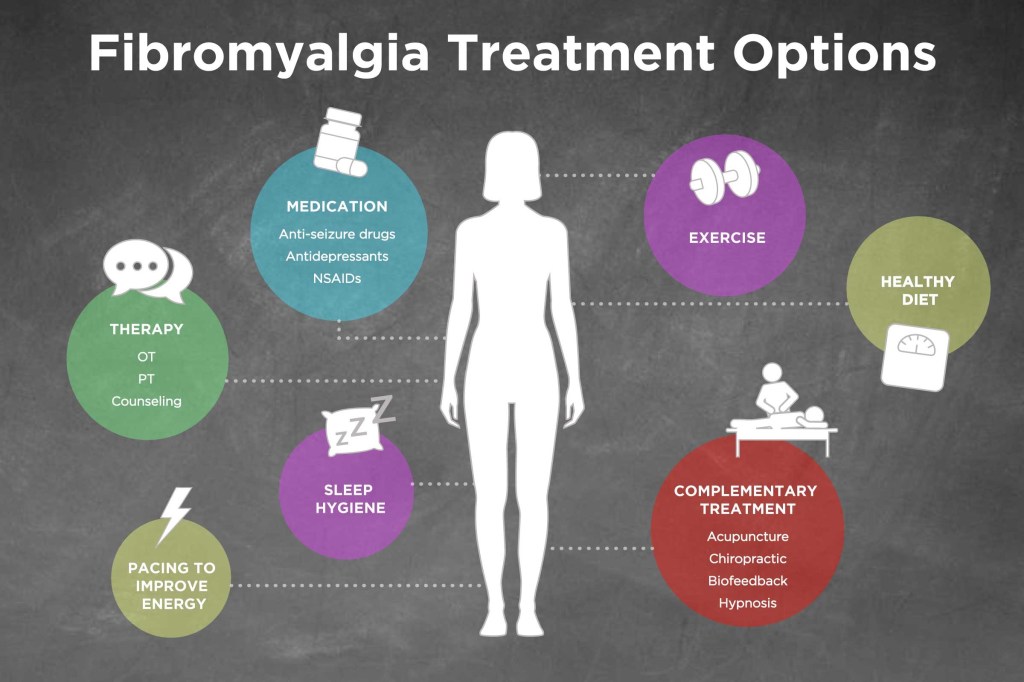
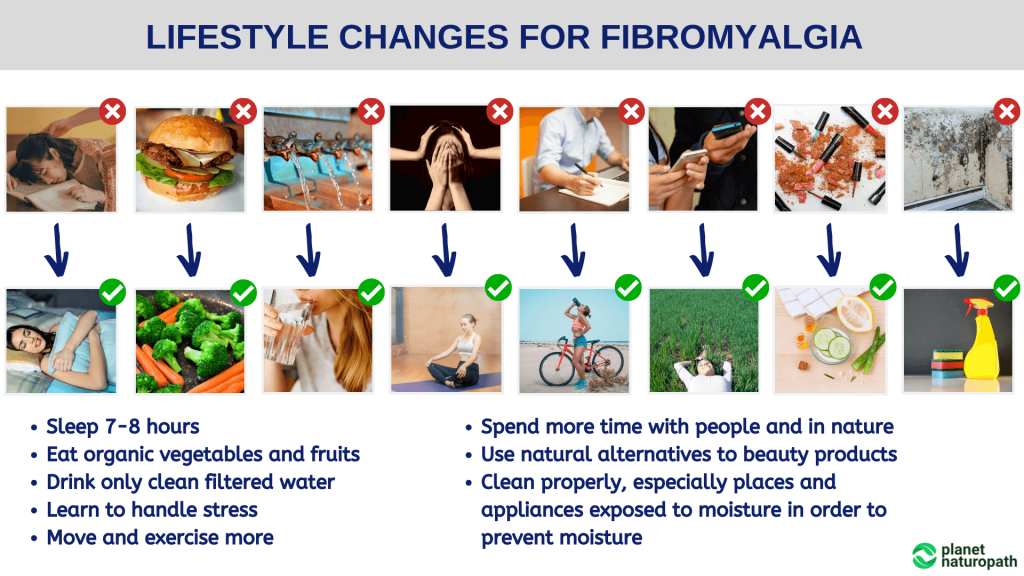
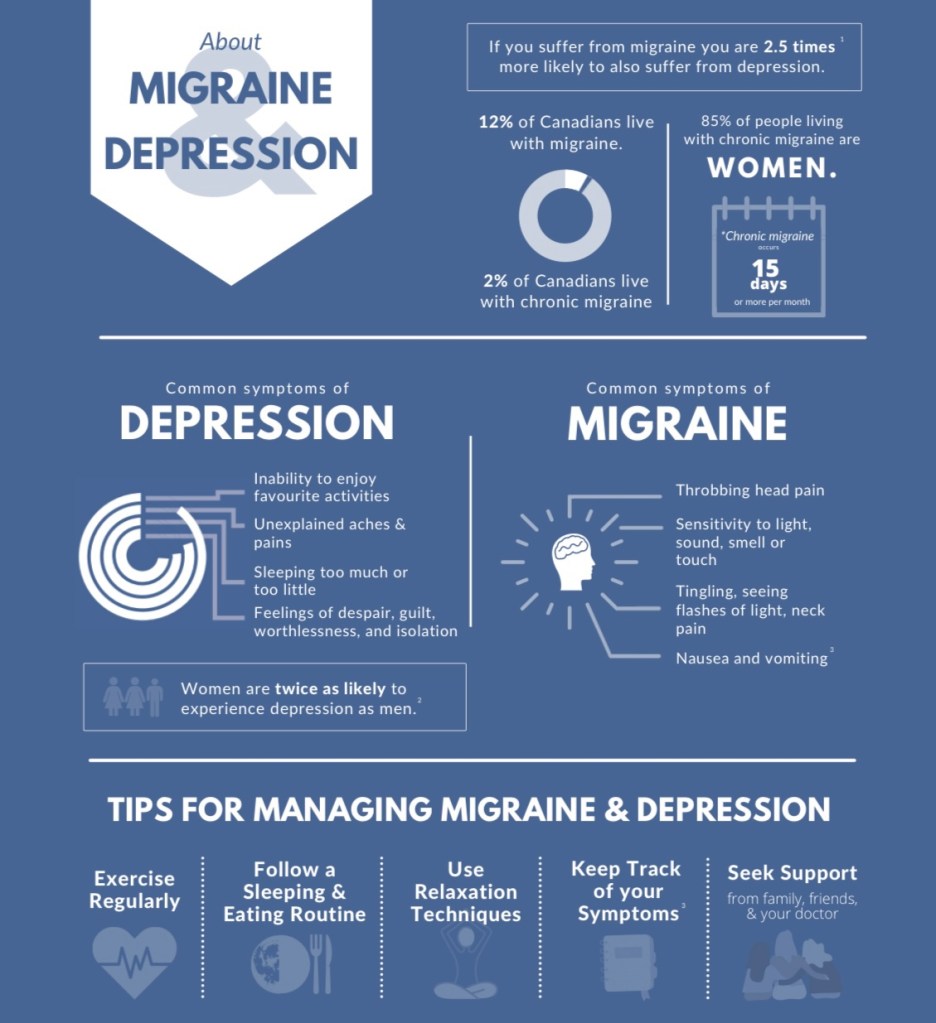
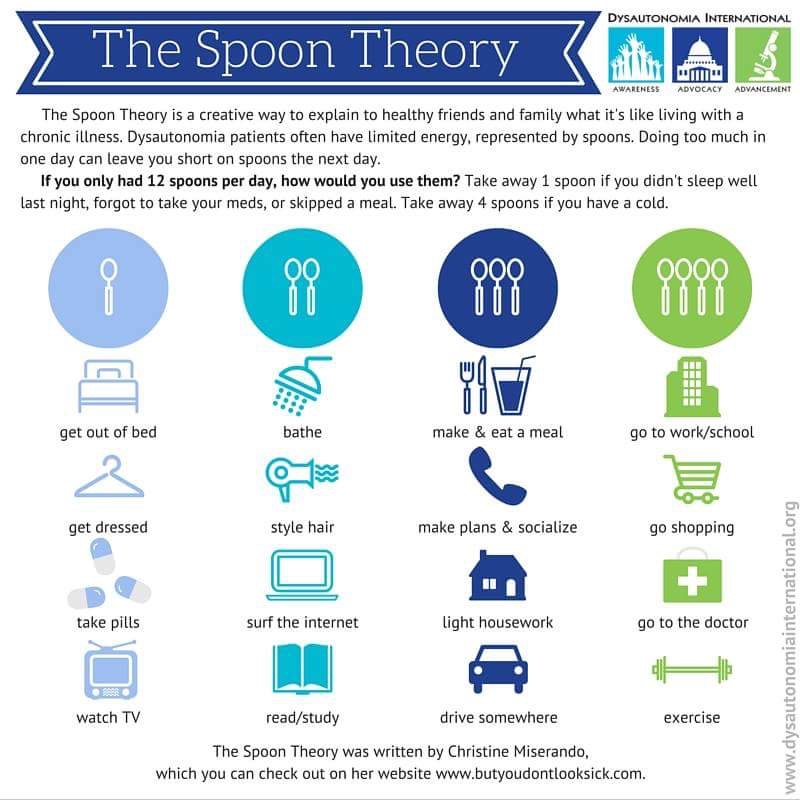
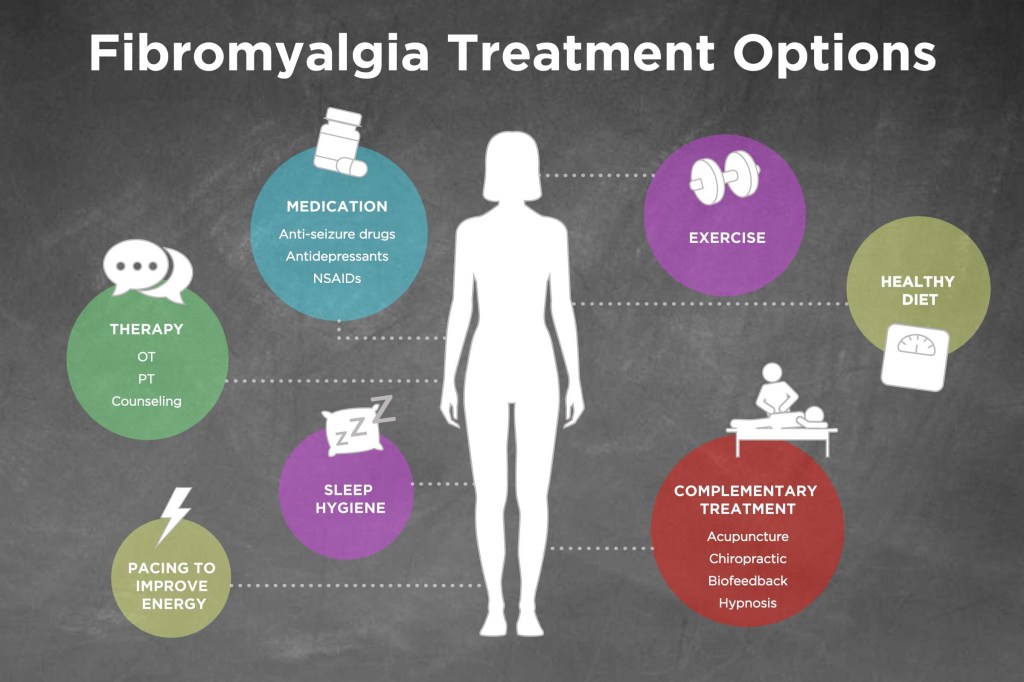
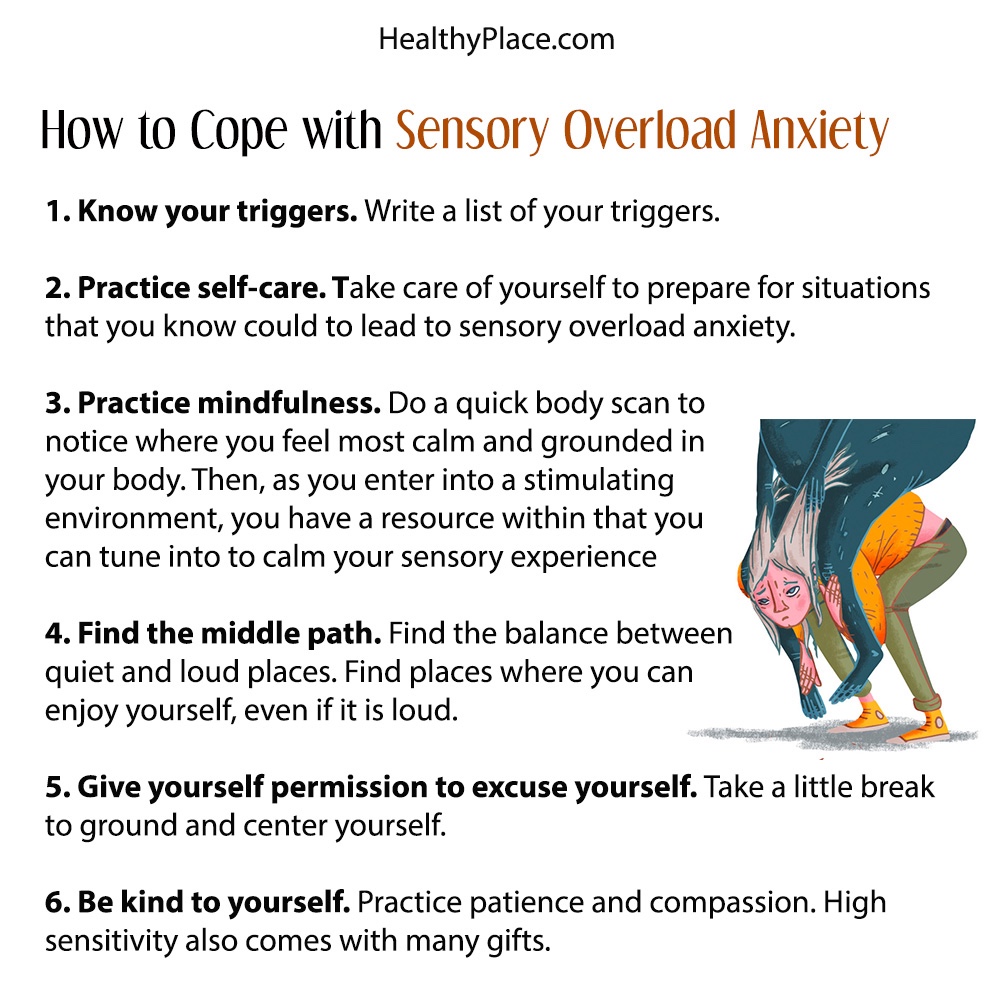
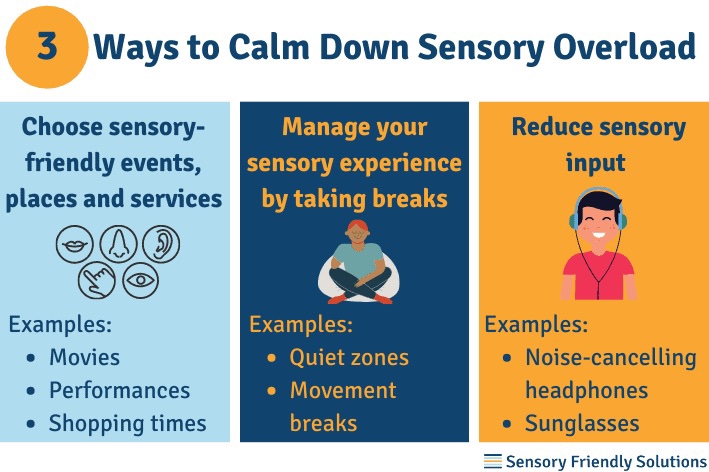
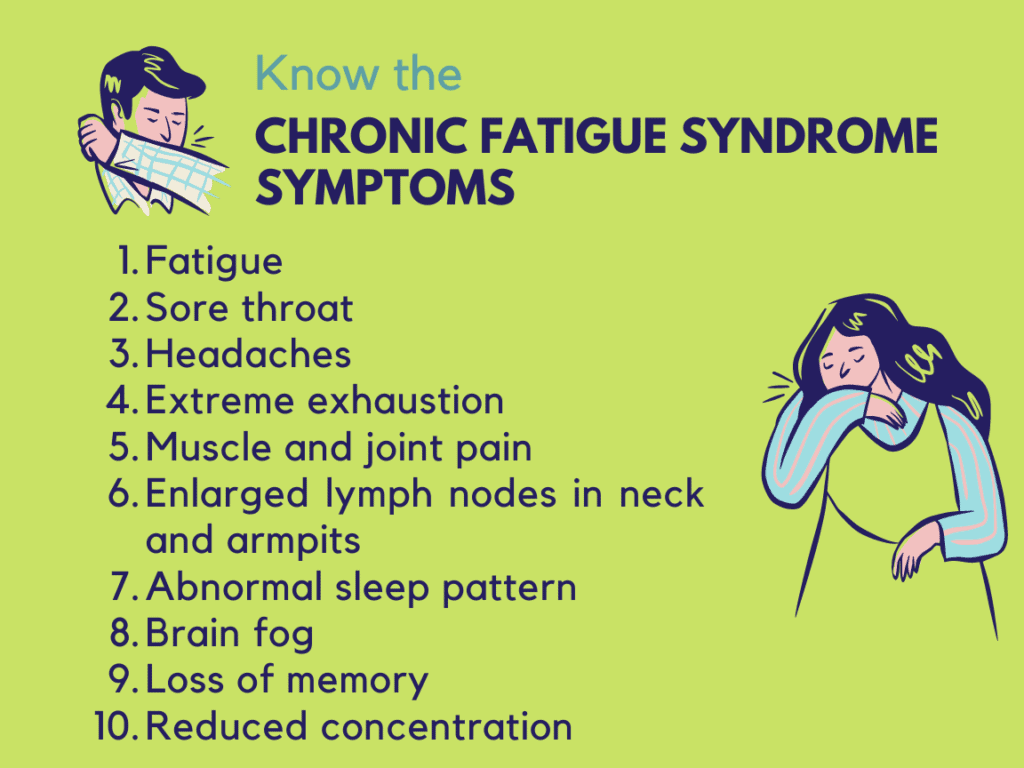
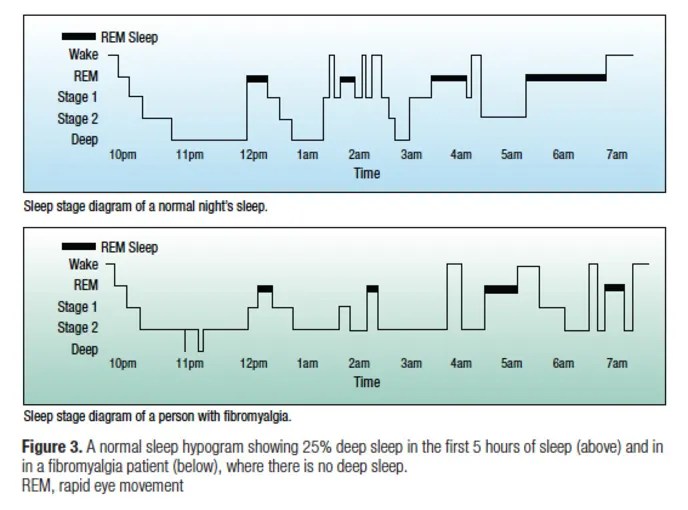
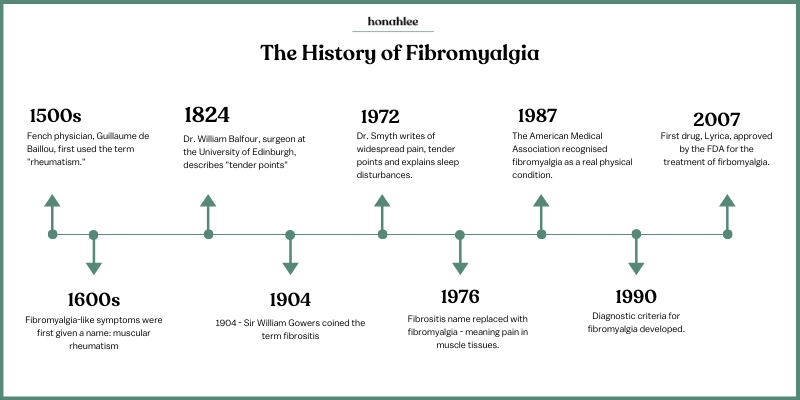
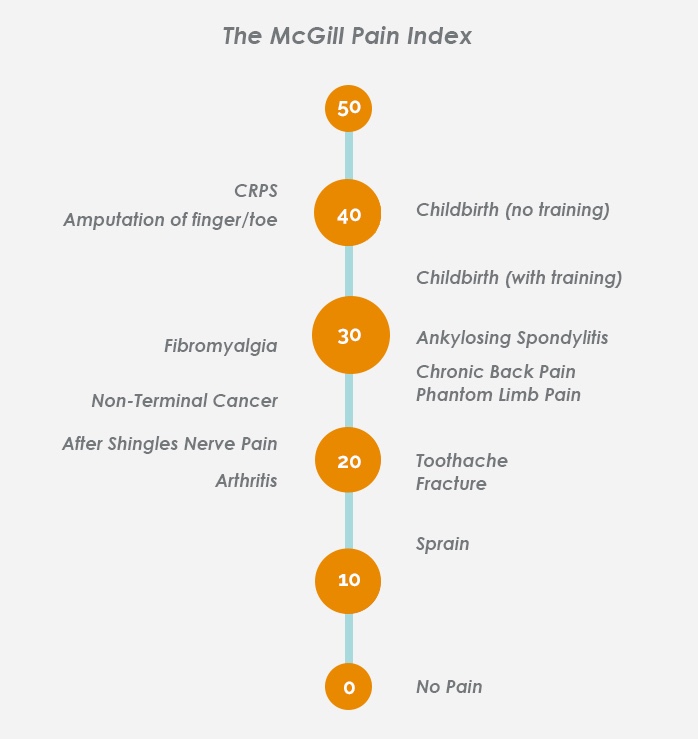
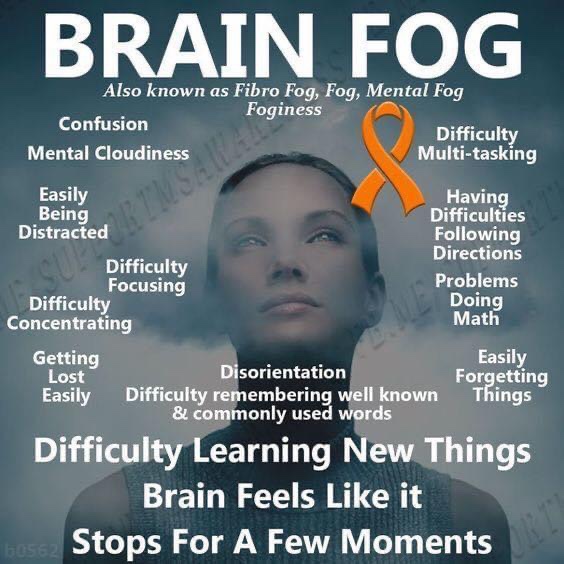
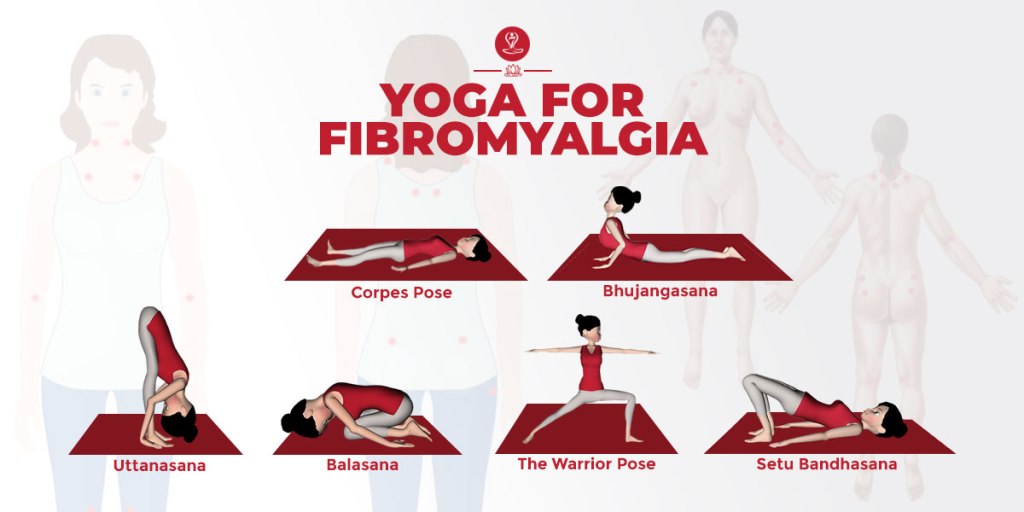
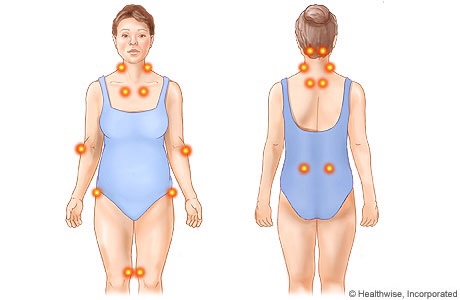
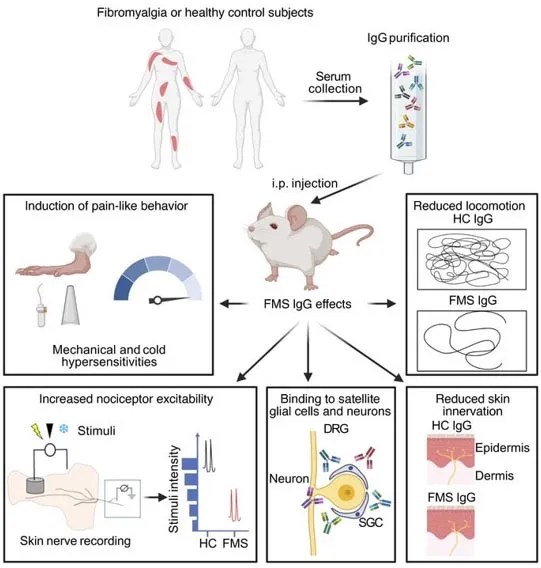
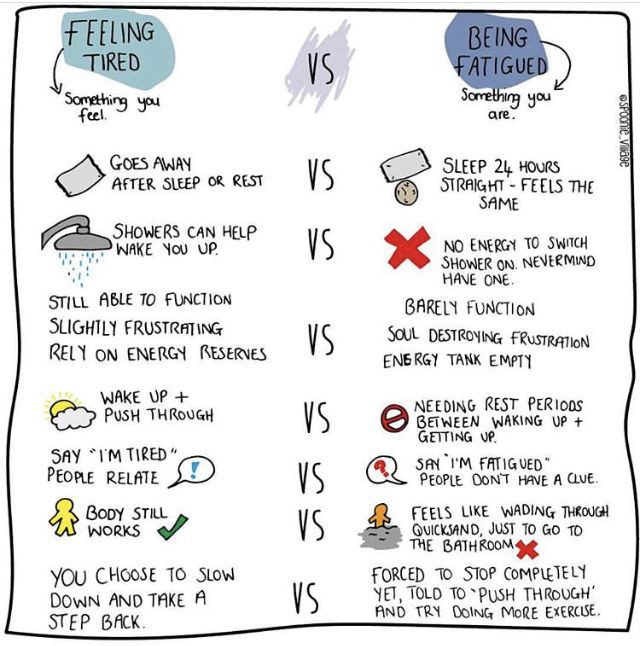
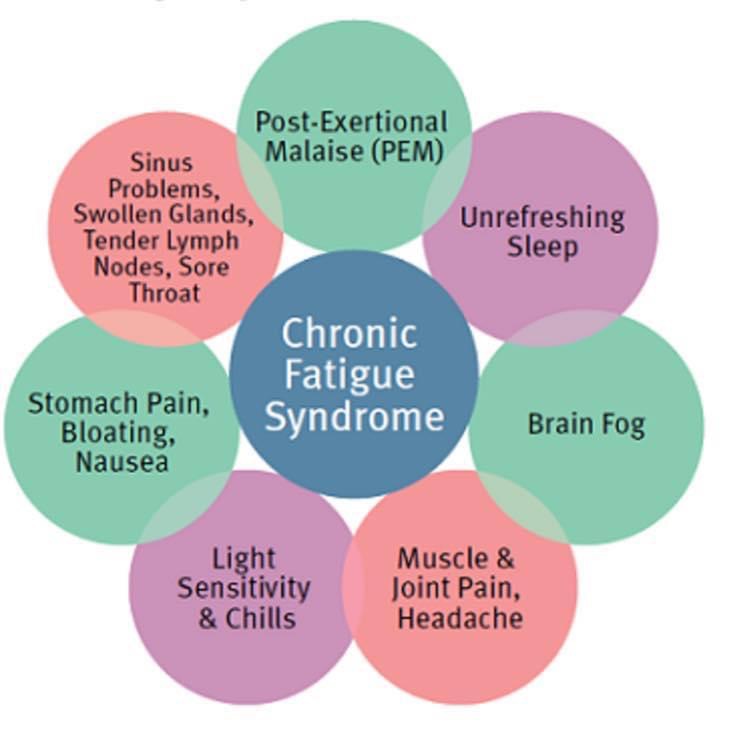
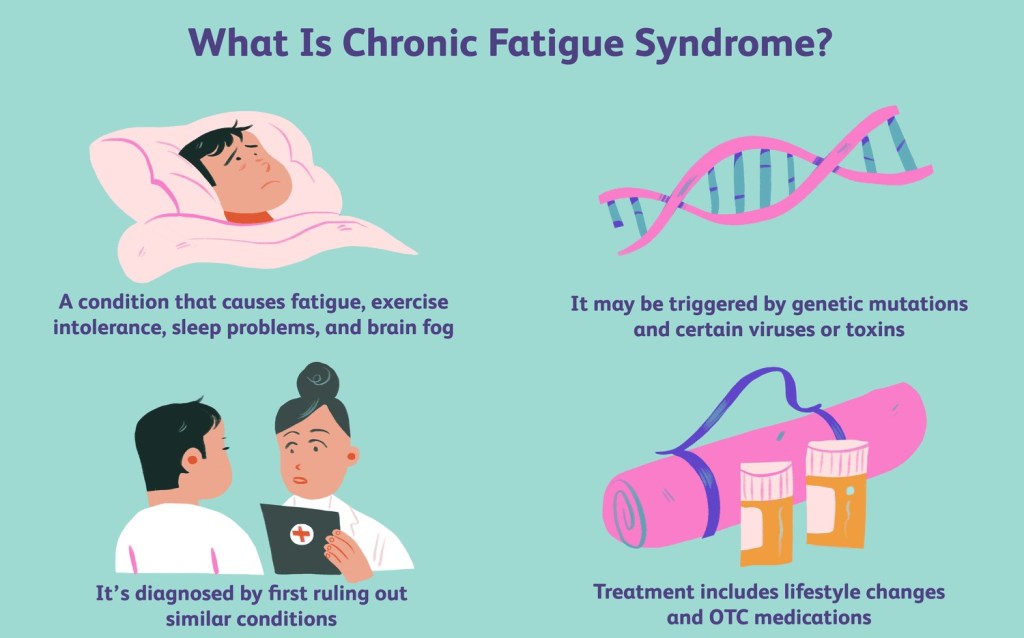
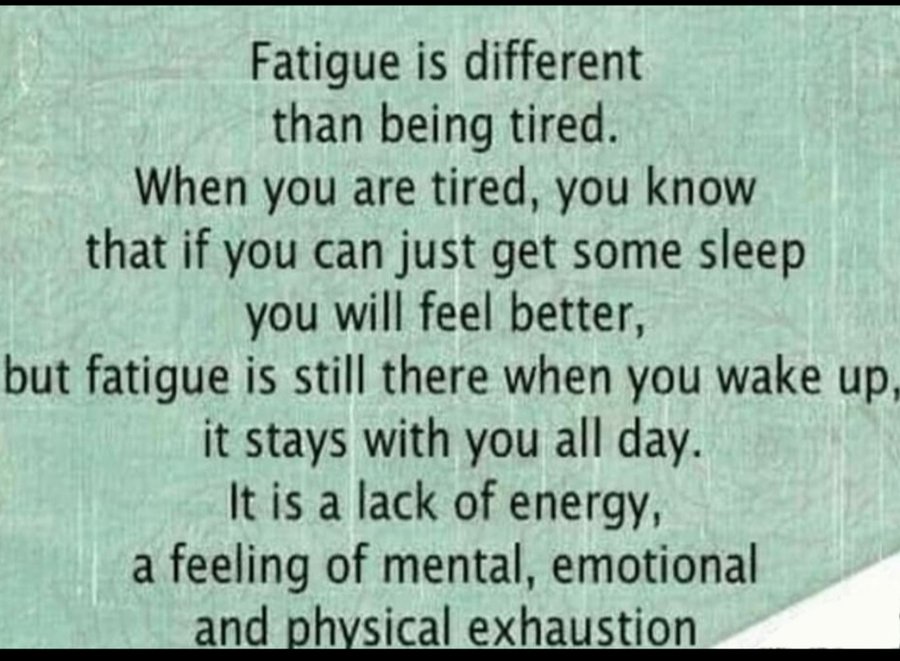
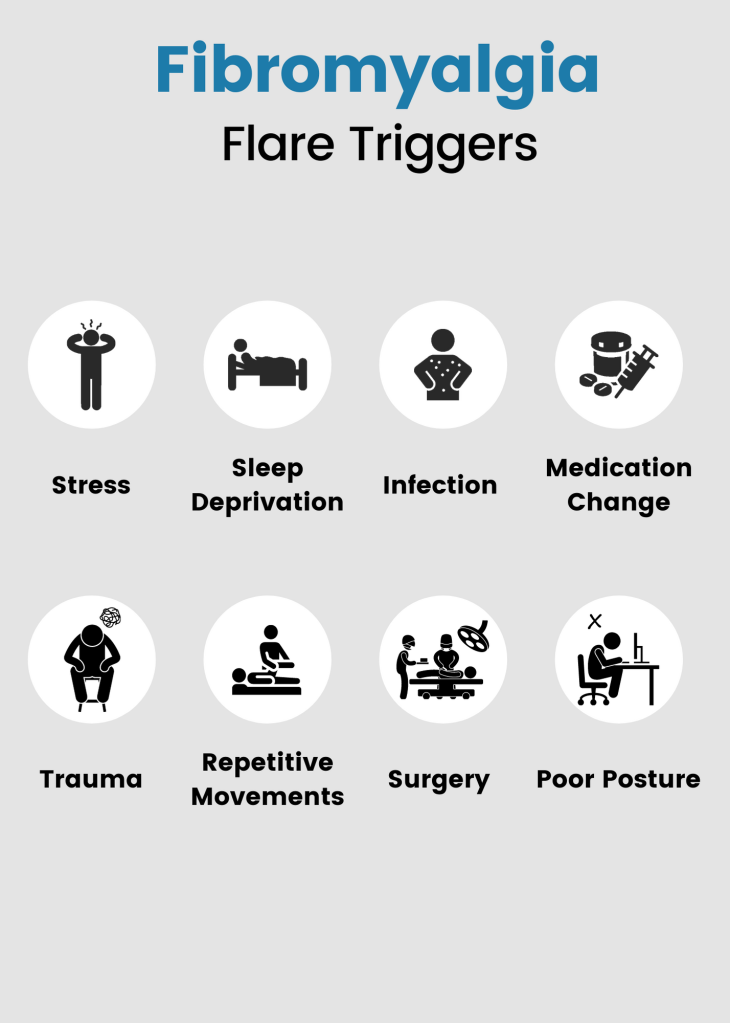
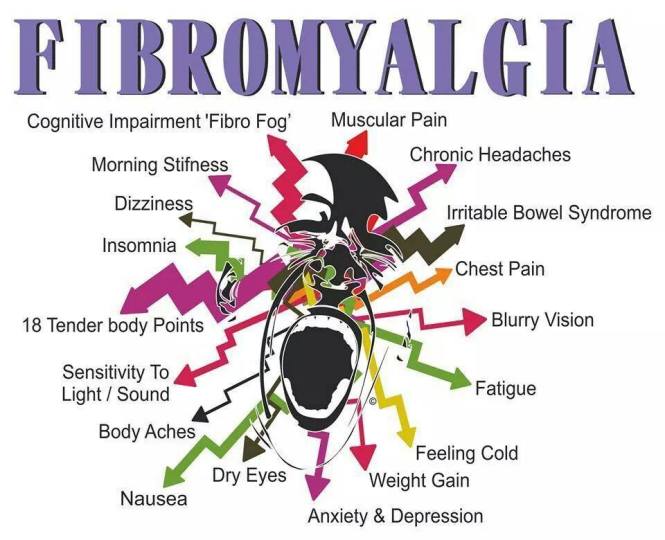
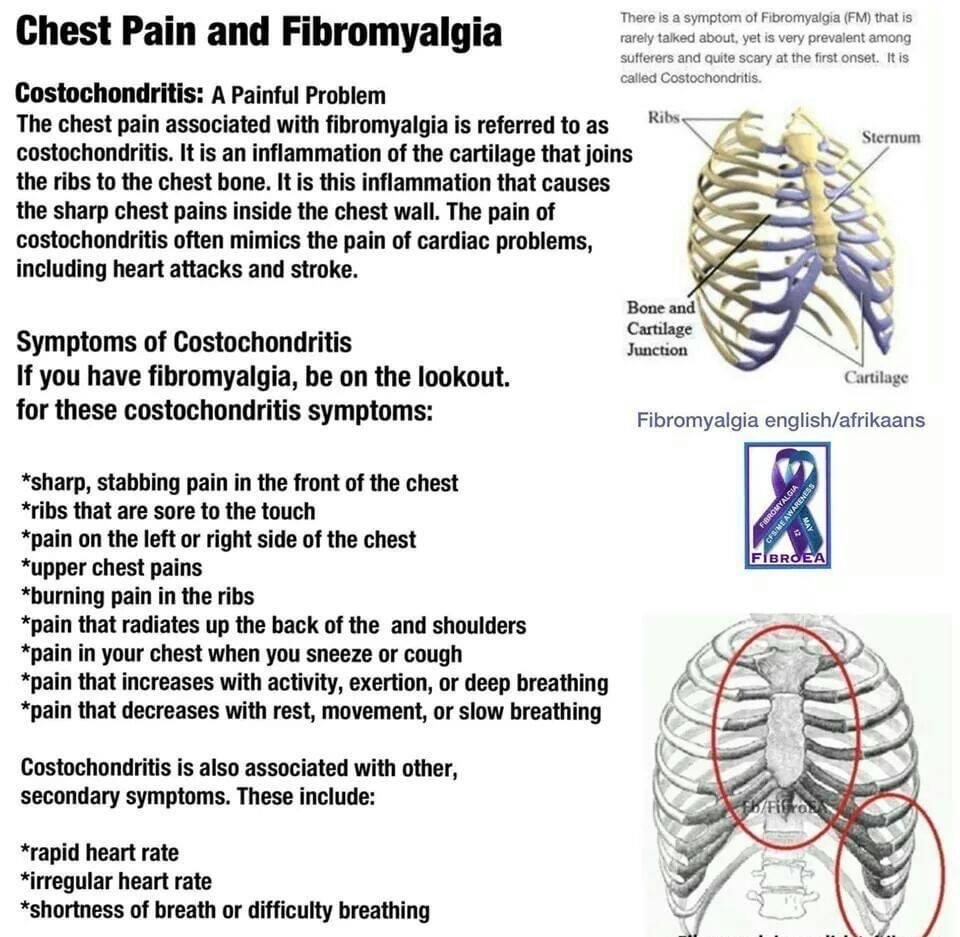
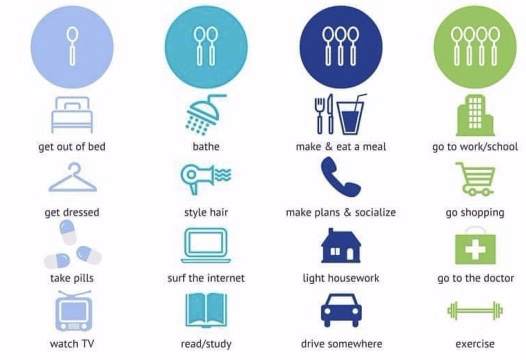
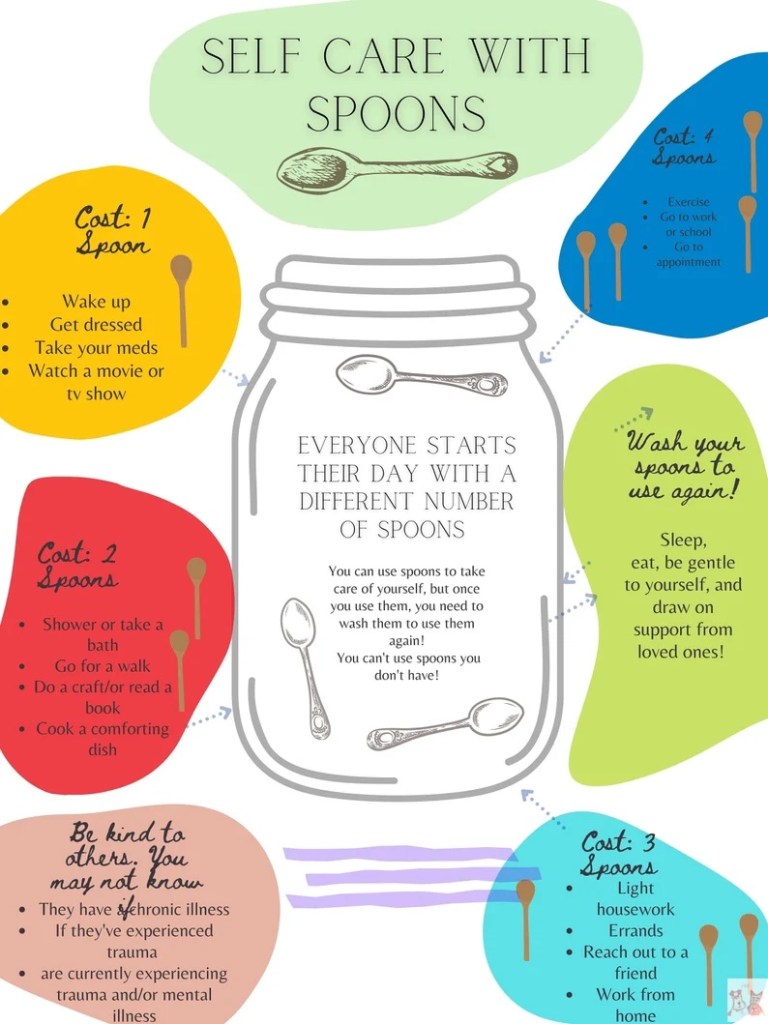
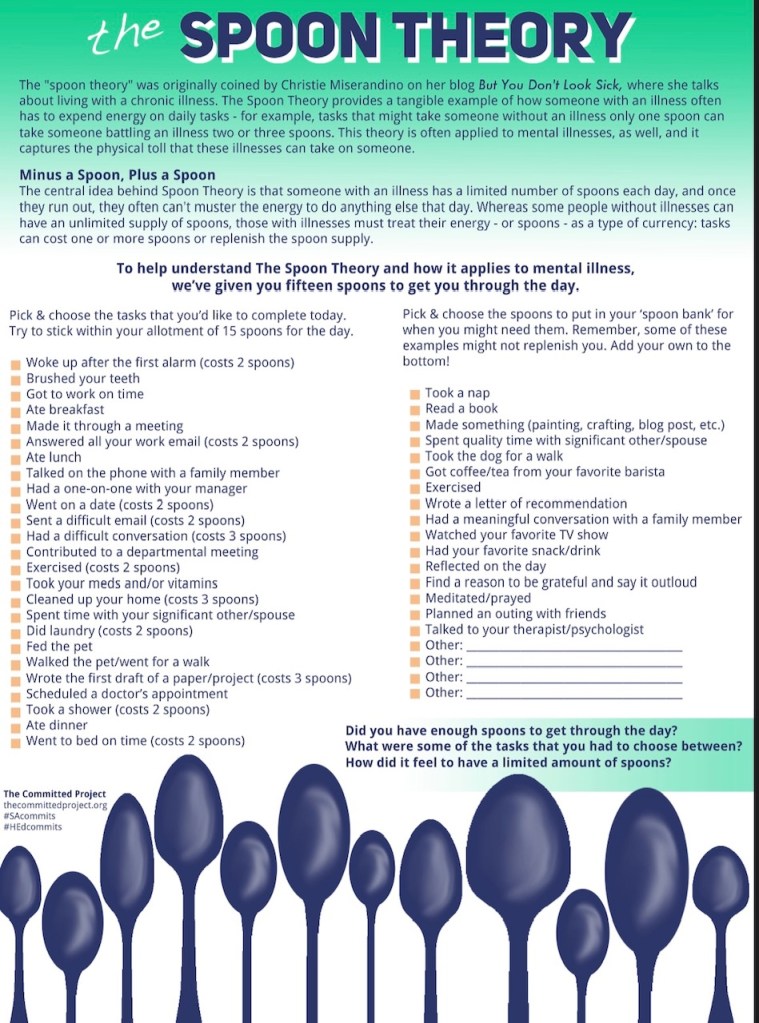
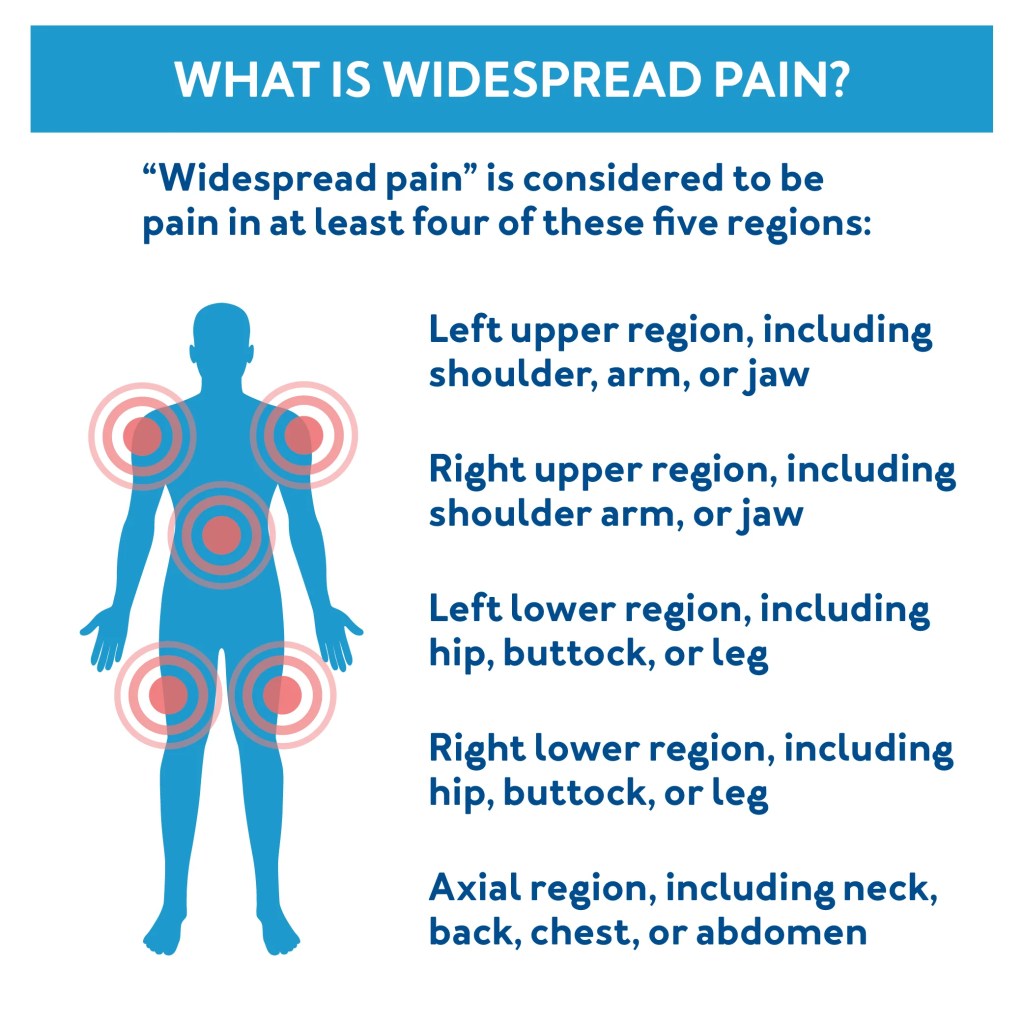
Over the last week, I have stepped back to reflect on this experience. How are we supposed to get proper treatment/help when so many medical providers do not think our health struggles/issues are valid and are labelled as controversial? Many medical providers world wide still believe fibromyalgia is not a legitimate condition and is often labeled as a mental illness. I wish I had some inspirational advice to give everyone, but I don’t. It is a frustration many of us face with invisible illnesses or misunderstood conditions.
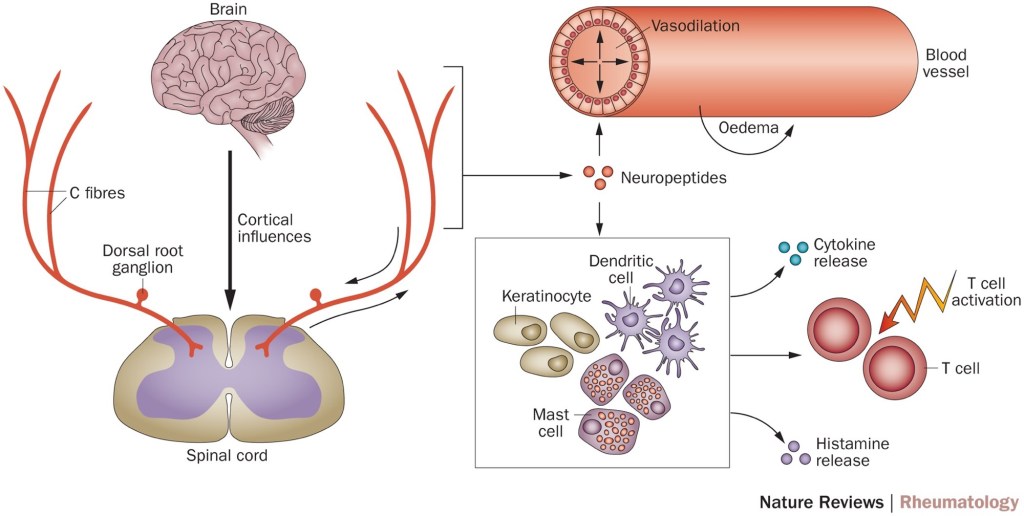
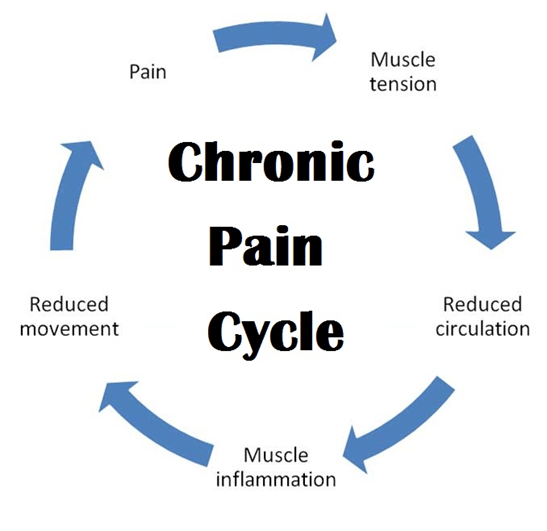
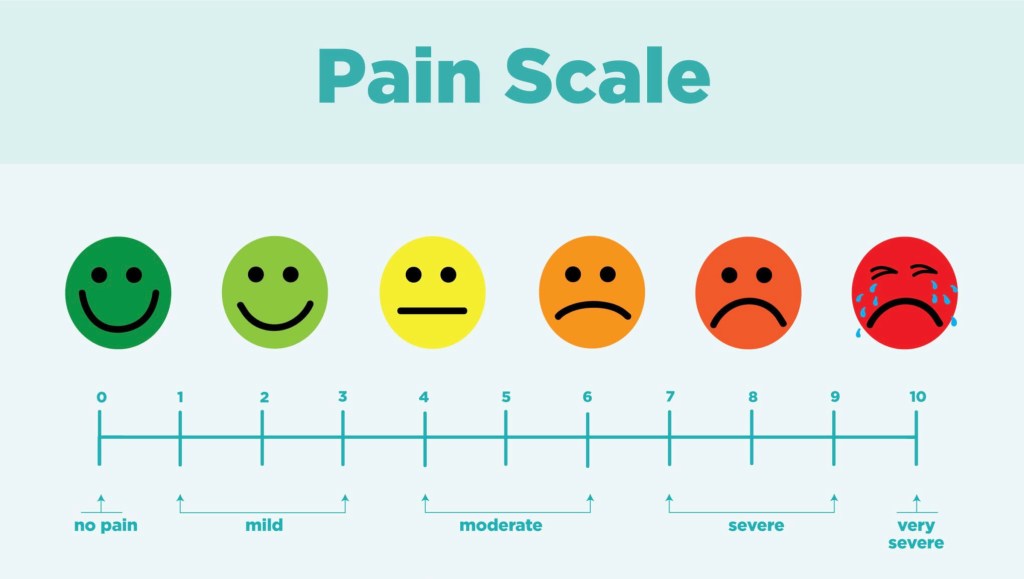
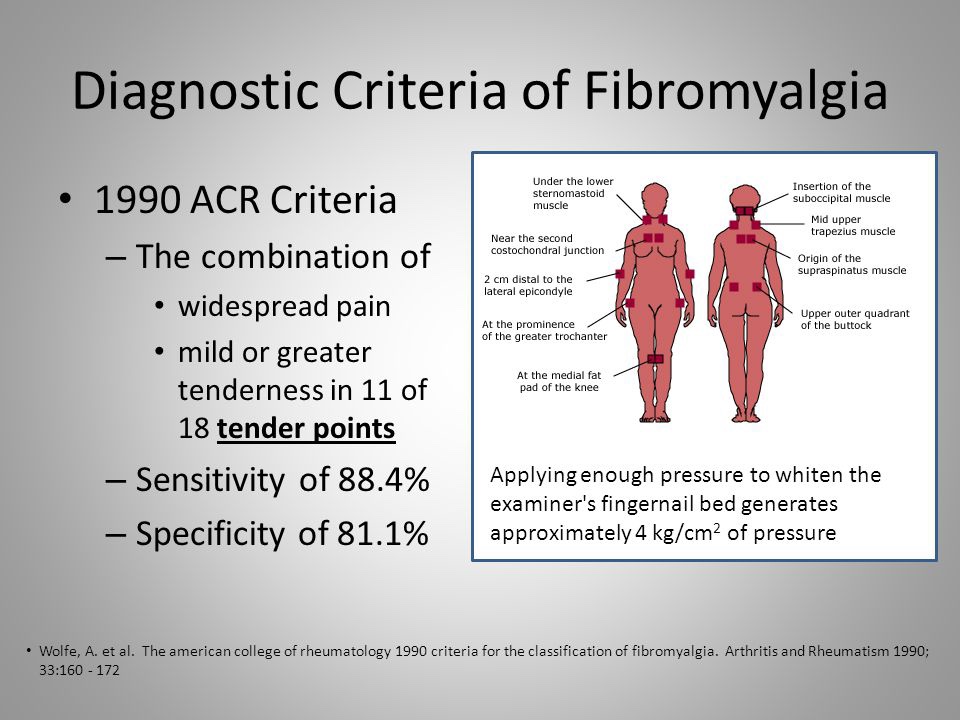
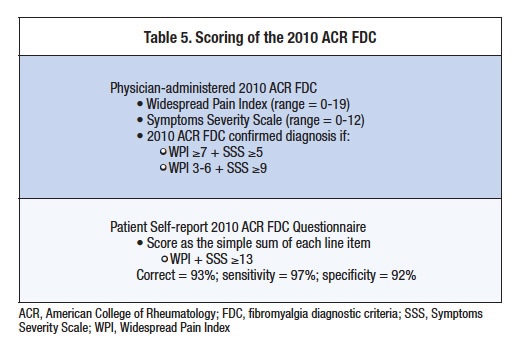
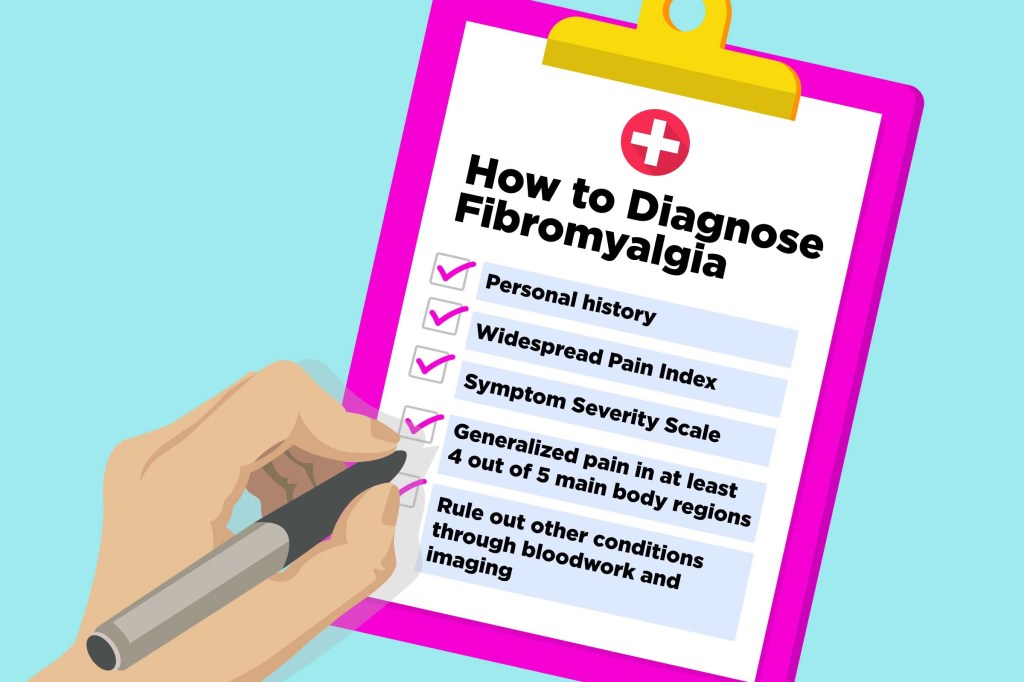
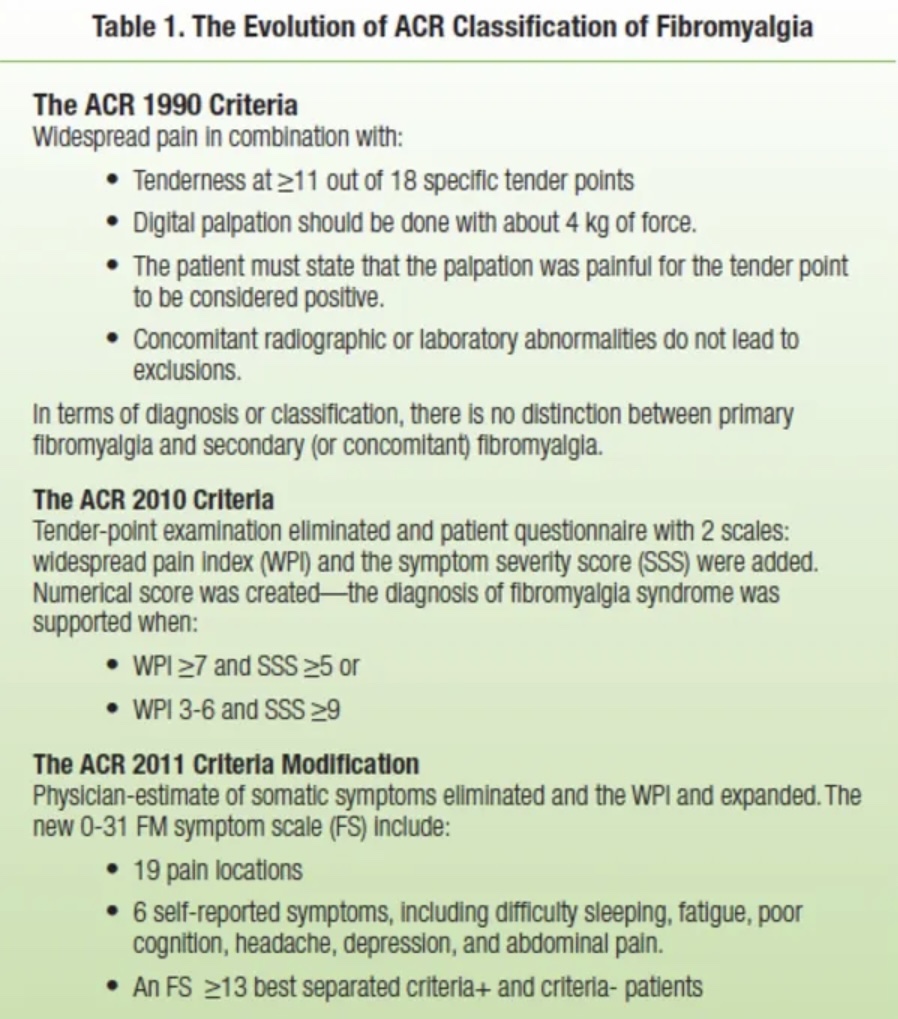
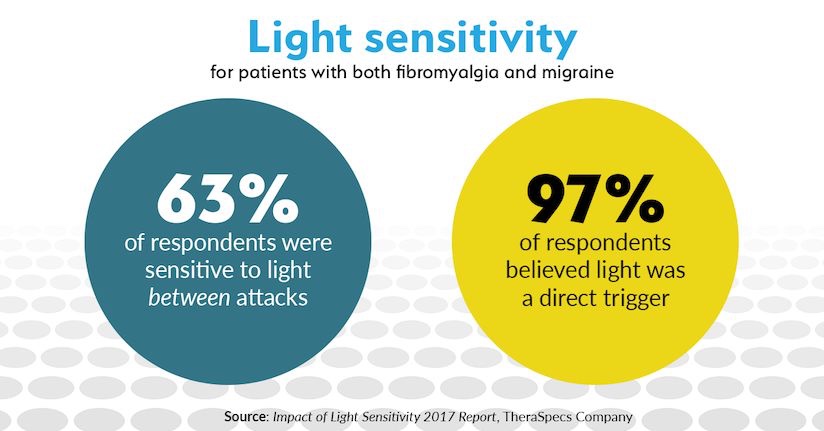
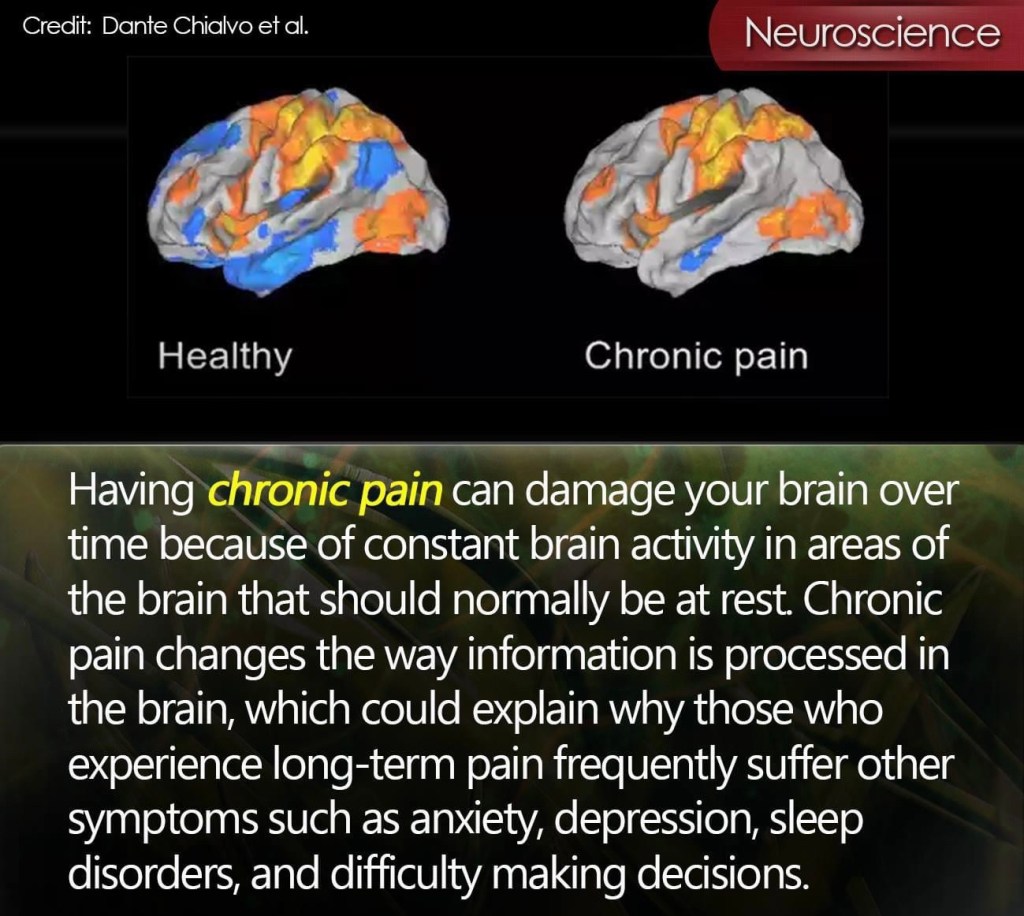
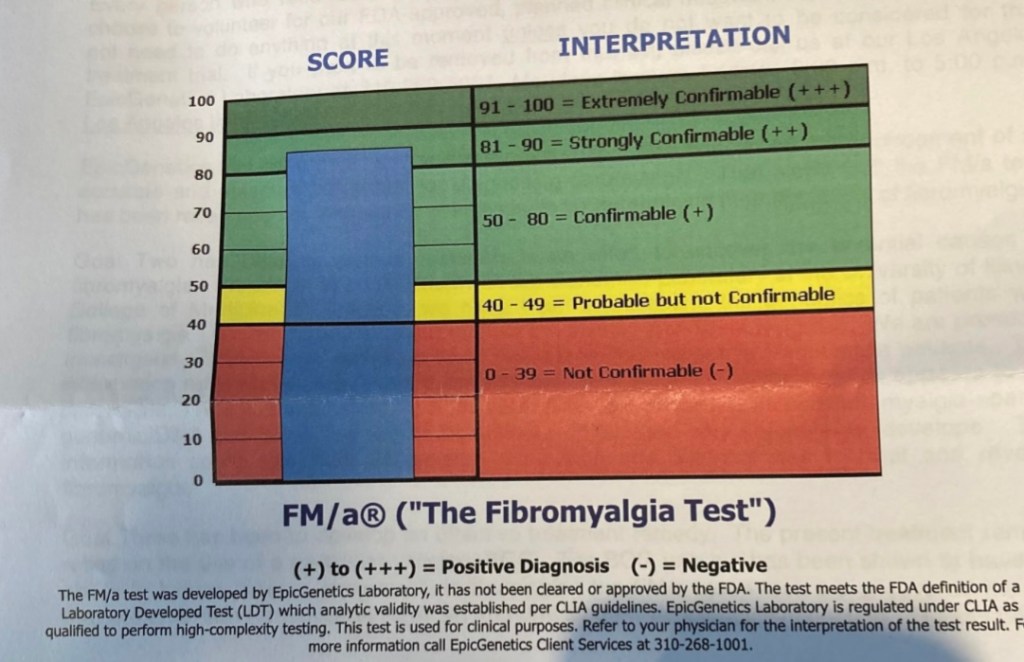
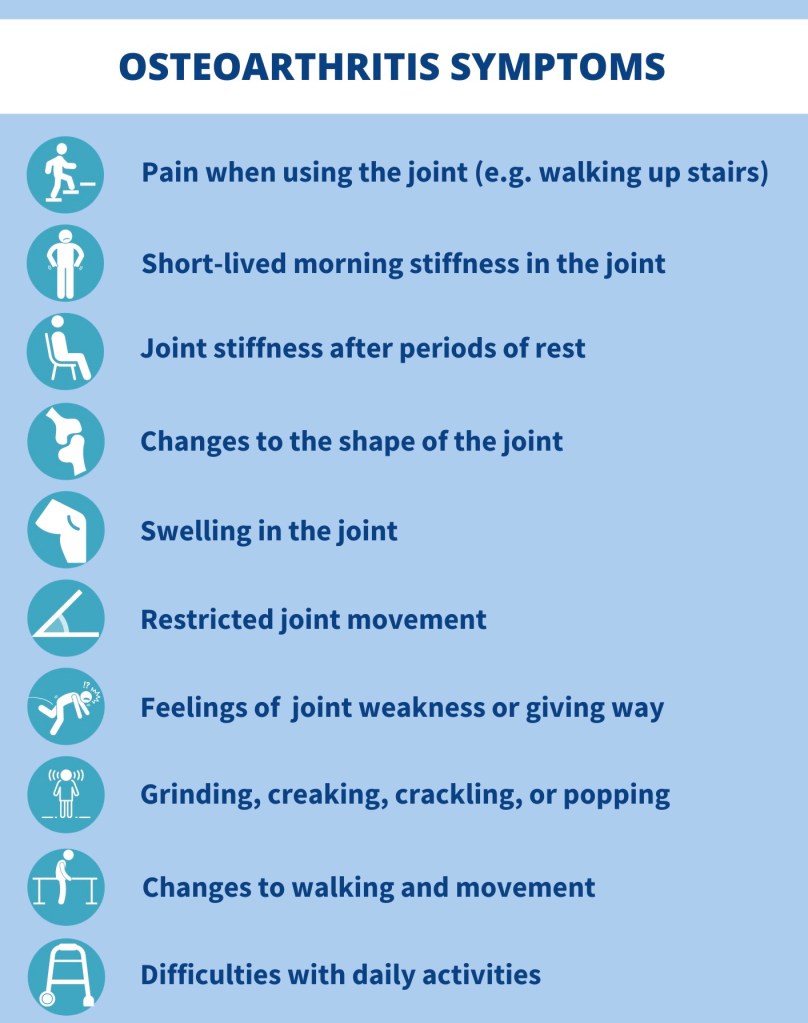
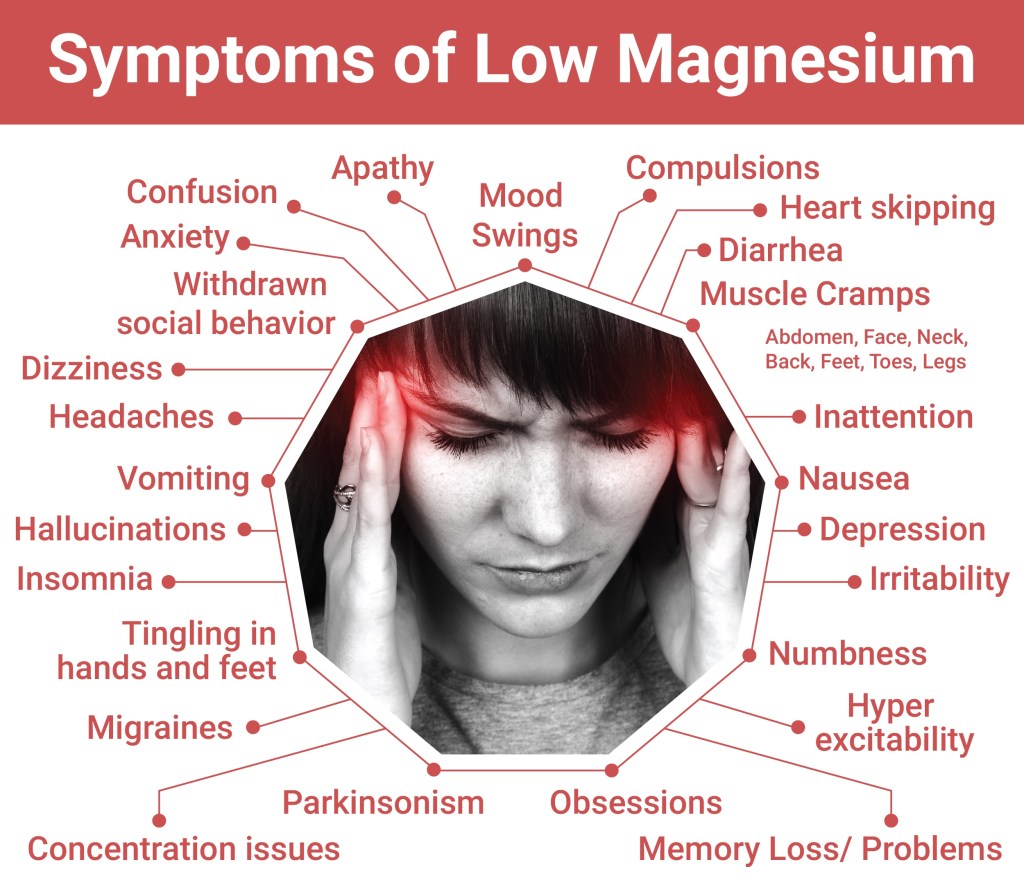
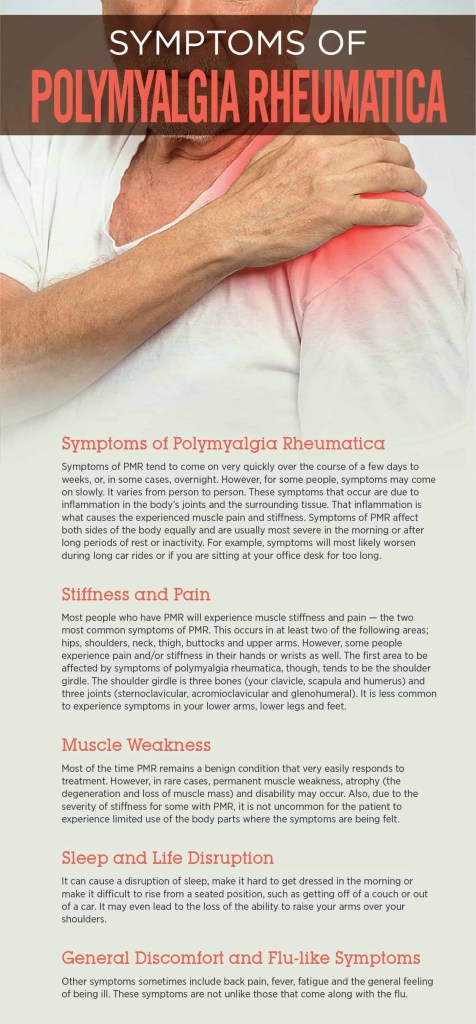
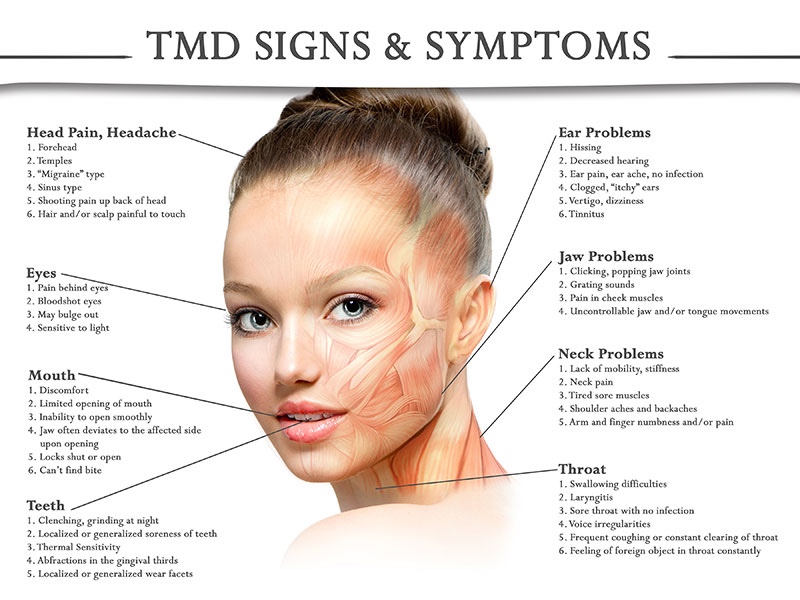
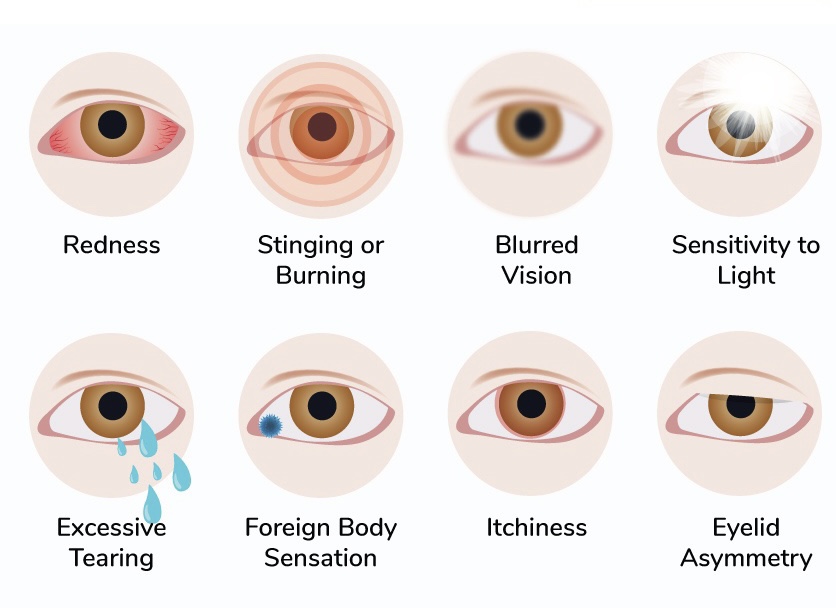
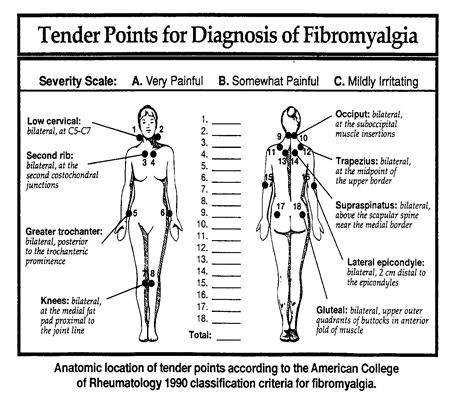
I often thought my fibromyalgia was diagnosed too quickly. Even though my doctor at the time was thorough in running tests, there were symptoms that just did not match a fibromyalgia diagnosis. These symptoms were left without an explanation for years. I eventually just “accepted” the fibromyalgia diagnosis and tried to move on with life managing symptoms – with little success. Symptoms got worse as did the intensity of the pain. I saw no positive changes, because lyme was the underlying cause of my pain and symptoms – most doctors are not trained to diagnose lyme or simply do not believe lyme disease is an issue. I do have fibromyalgia, but the lyme diagnosis was the missing link.

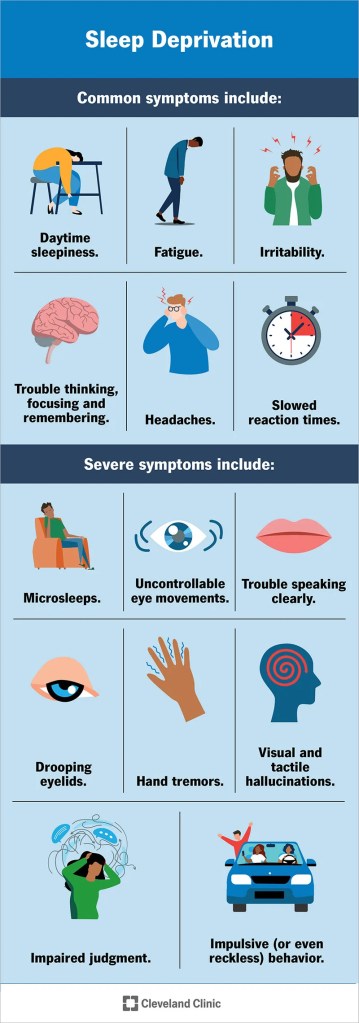
When medical professionals fail to understand a condition or simply do not believe a condition exists the following may take place:
- Being misdiagnosed with the wrong conditions.
- With the misdiagnosis – insufficient support and improper treatment .
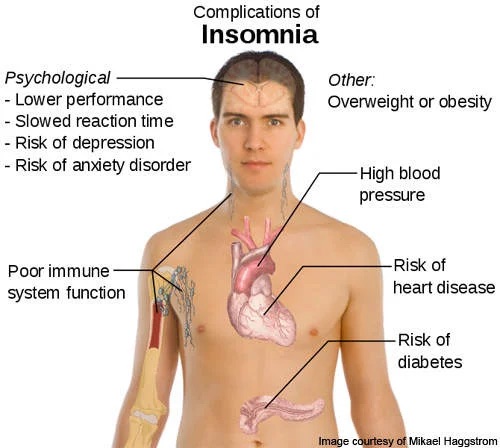
- Health consequences. People continue to get sicker because because of delayed treatment.
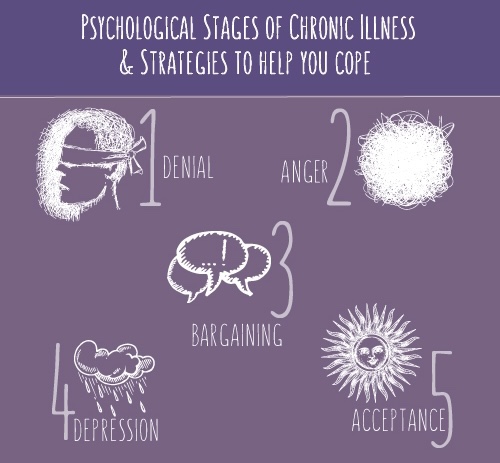
- Psychological distress
It is hard for me not to think..
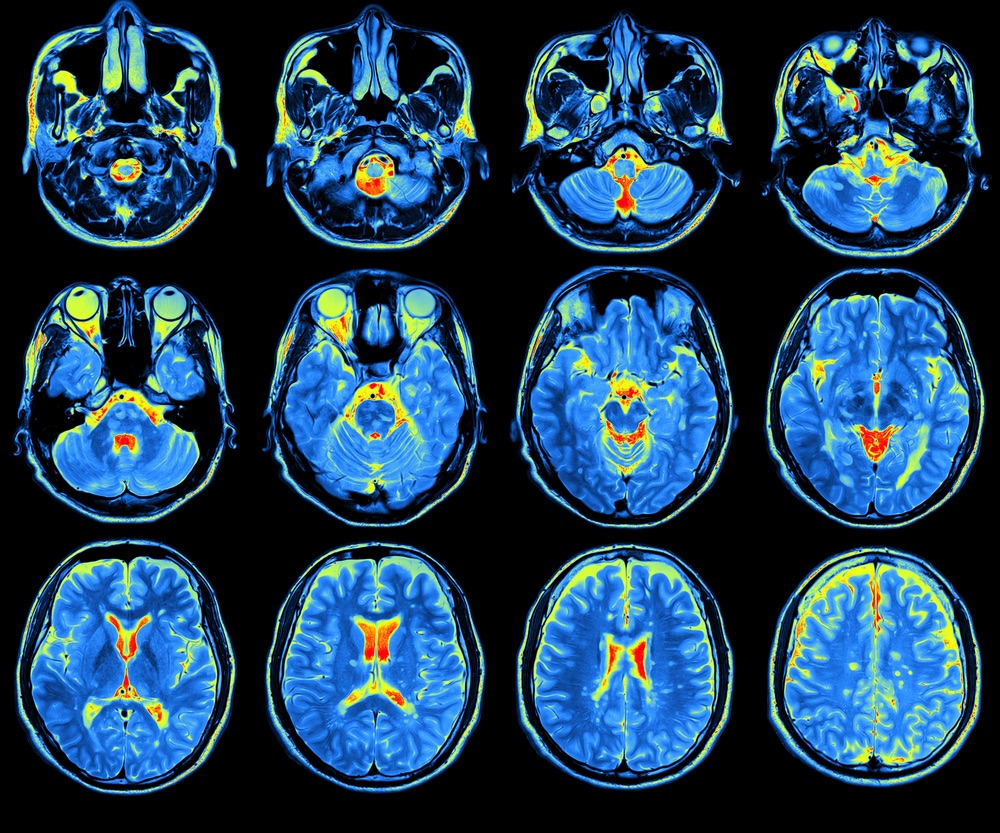
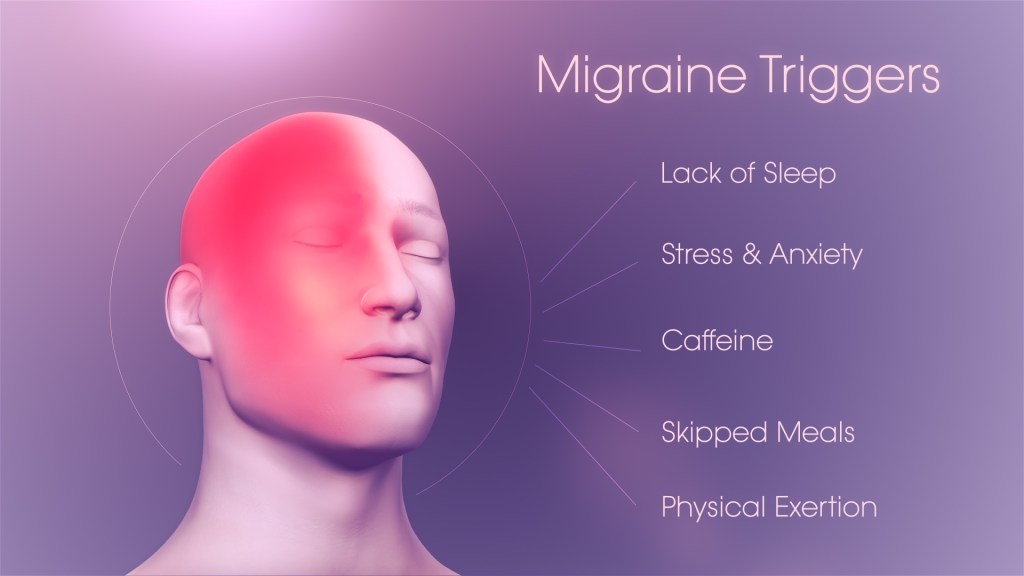
1 “If only the lyme had been caught sooner, I wouldn’t have become so sick!” The longer lyme is left untreated the more damage it can cause to one’s body head to toe. It can cause damage to vital organs if left untreated. This week I go for for an ultrasound on my heart to make sure the lyme bacteria has not entered into the layers of my heart muscles – it is known to cause an enlarged heart.
2. ” If only I had reached out to the naturopathic doctor (ND) sooner, instead of repeating the same lab tests over and over which all reflected normal. A friend of mine had given me the ND’s contact information two years prior to me actually reaching out to her. I wish I had done so way sooner.
3. The doubt from some medical providers ( not all) contributed to my anxiety disorder. If I had to see a doctor who was unfamiliar with my file, they would immediately blame the symptoms on anxiety. I’ve also been told by several health providers I was not trying to get better.
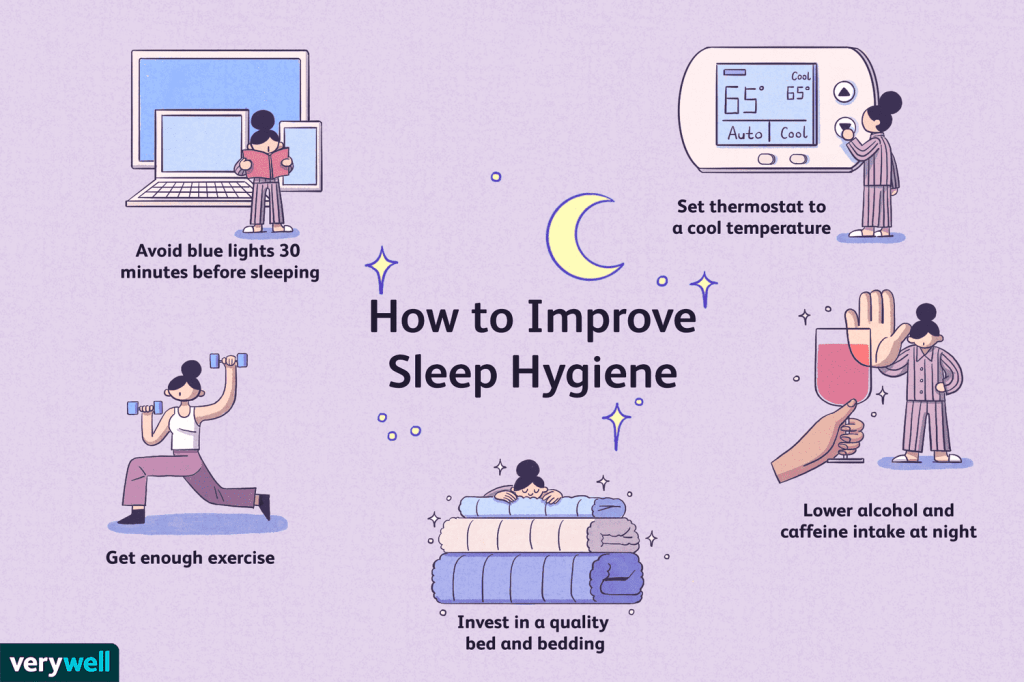
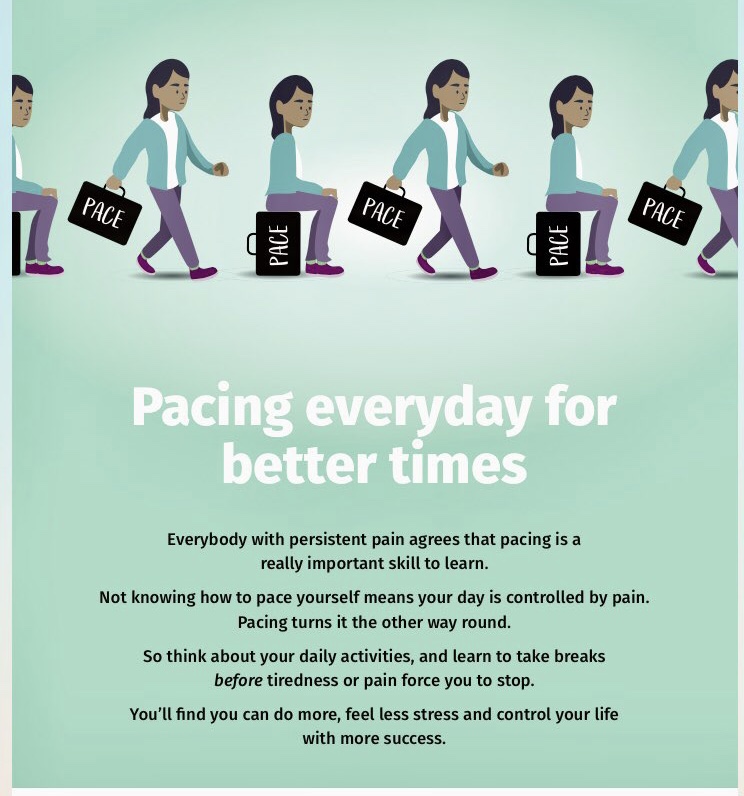
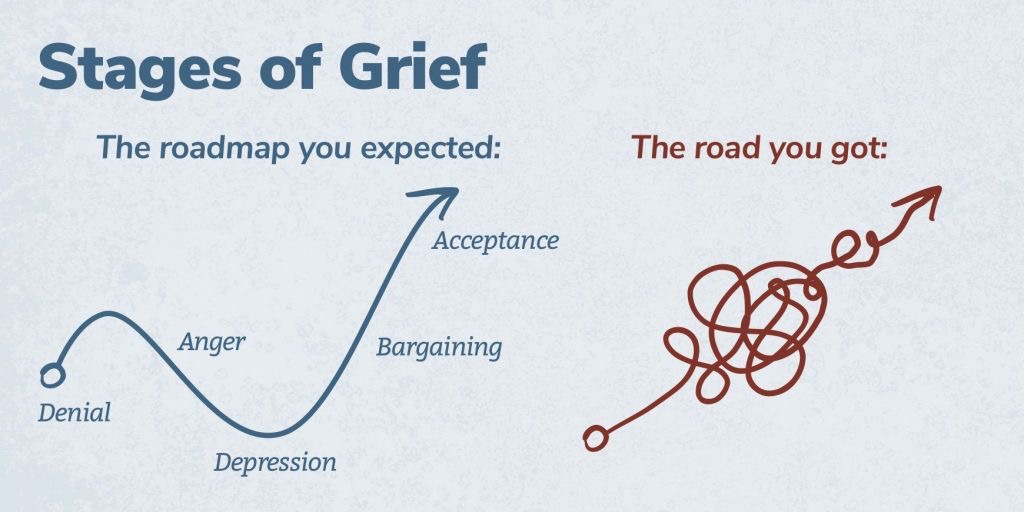
I am working on not focusing on the what ifs, as I can’t change what took place. All I can focus on is what is in front of me now – today. The what ifs were only contributing to my anxiety levels – increasing symptoms and making me sicker.