Before I got diagnosed with fibromyalgia my vitamin levels were perfectly normal. As the years pass, my vitamin levels continue to drop. I do know aging can causes our vitamin levels to be lower, however I believe fibromyalgia has played a part in my vitamin levels dropping fairly low. Research actually proves fibromyalgia can lower certain vitamins in the body, which may make fibromyalgia symptoms worse. There are actually theories out there that vitamin deficiencies are partially responsible for fibromyalgia development. I recently had blood work done and a I have learned a lot of my vitamin levels are extremely low.

Iron
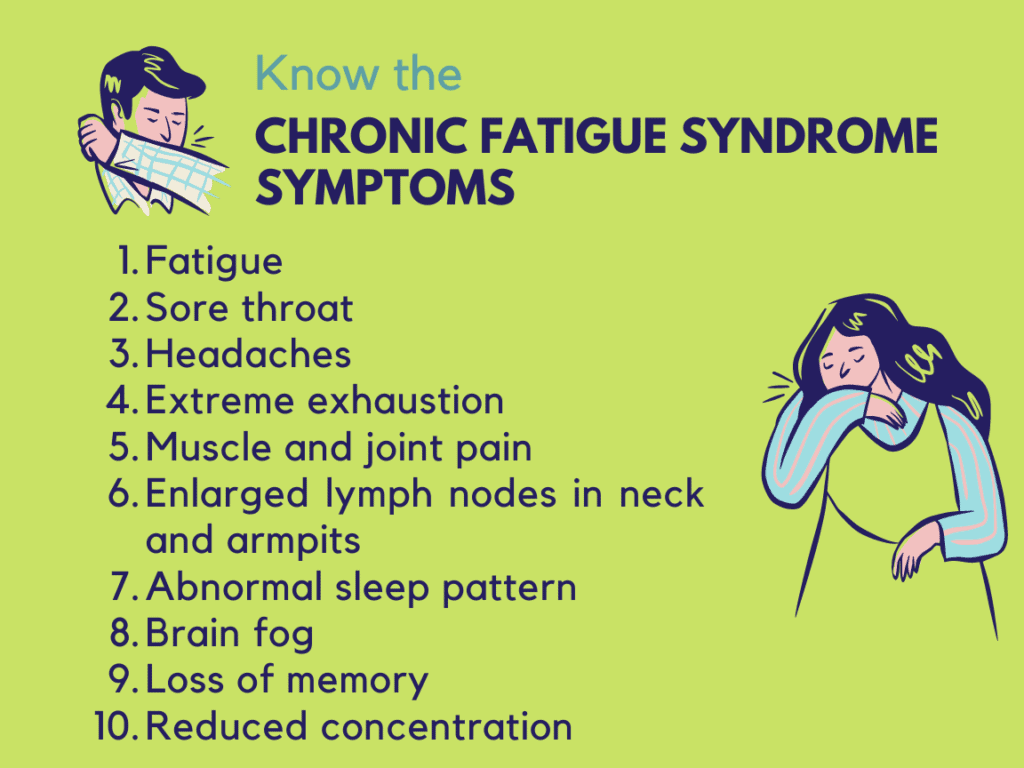
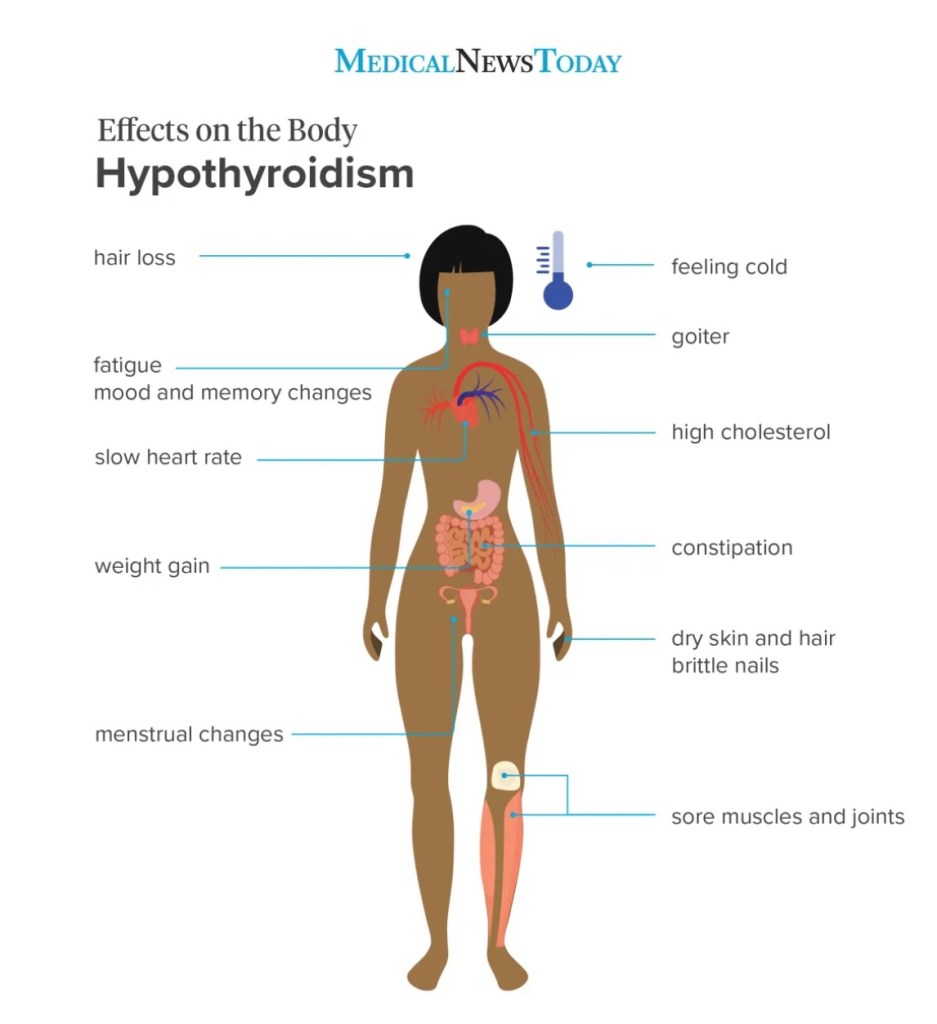
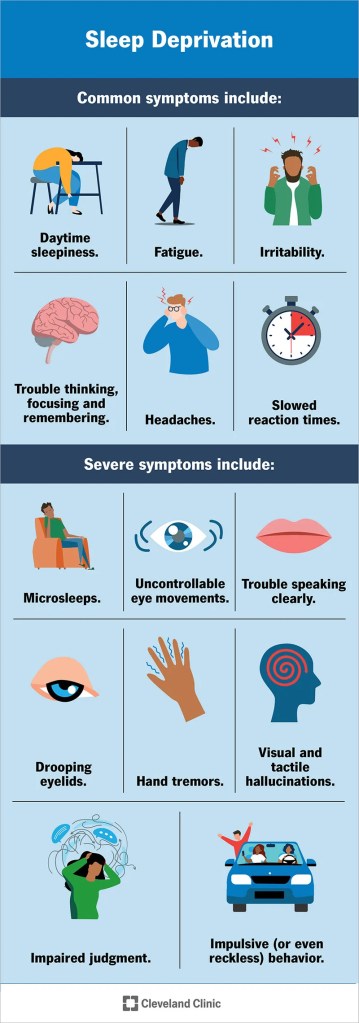
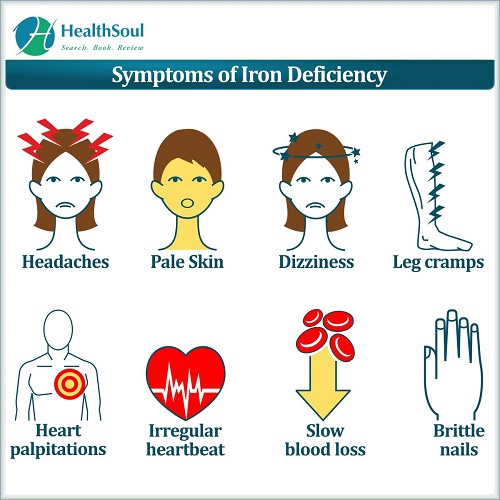
Having low iron levels can either mimic or possibly contribute to heightened fibromyalgia symptoms. Women with fibromyalgia are more likely to have iron deficiency. Low iron can cause extreme fatigue to form. For those of us with fibromyalgia the chronic fatigue, muscle/joint pain, headaches, weakness, further decreases endurance levels and sleep disturbances may all heighten, as low iron levels can cause all theses symptoms to arise. Having low iron can also cause a person’s pain threshold to lower and increasing pain sensitivities! I’ve had lower iron levels for some time now, even with iron supplements. I now wonder if low levels of iron are causing some of my fibromyalgia symptoms to feel worse.
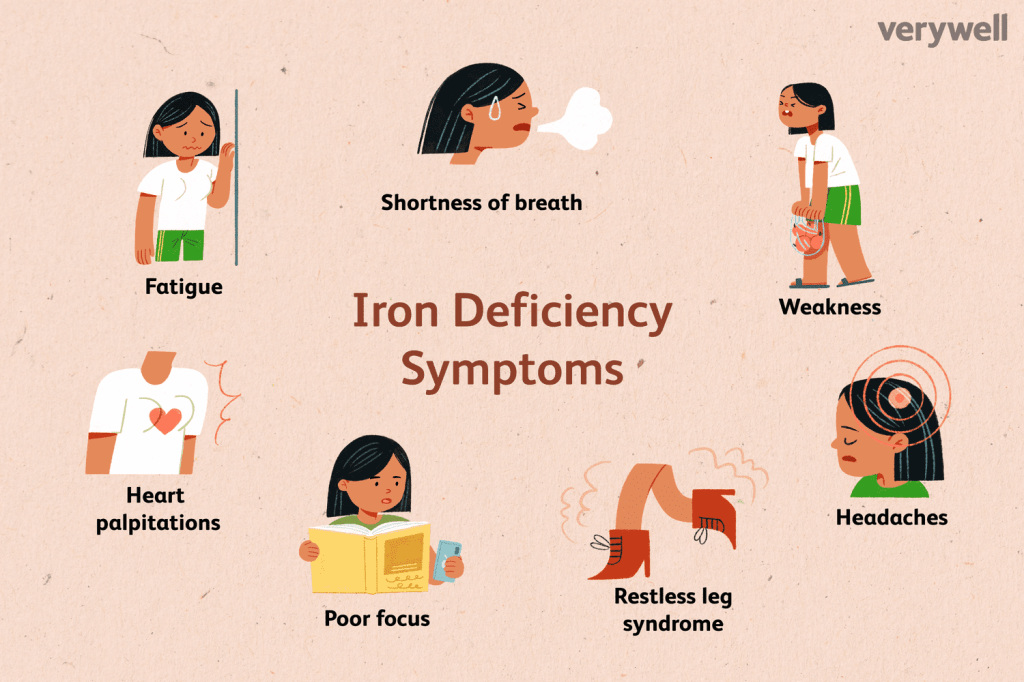
A study done in 2010, revealed that there appears to be an association between ferritin levels and fibromyalgia. People with fibromyalgia tend to have lower levels of ferritin then those without fibromyalgia. Ferritin is responsible for storing iron in the body. For myself my ferritin level has remained stable. This study is older, but as far as I know there has been no current study done. Here is the link for the study.
You can read more about iron deficiency here.
Calcium
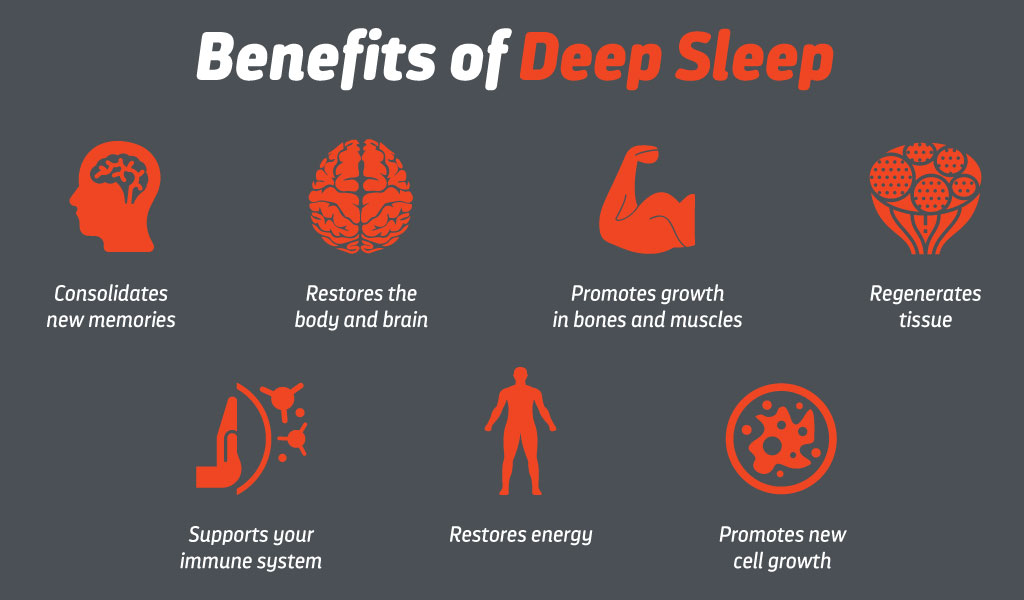
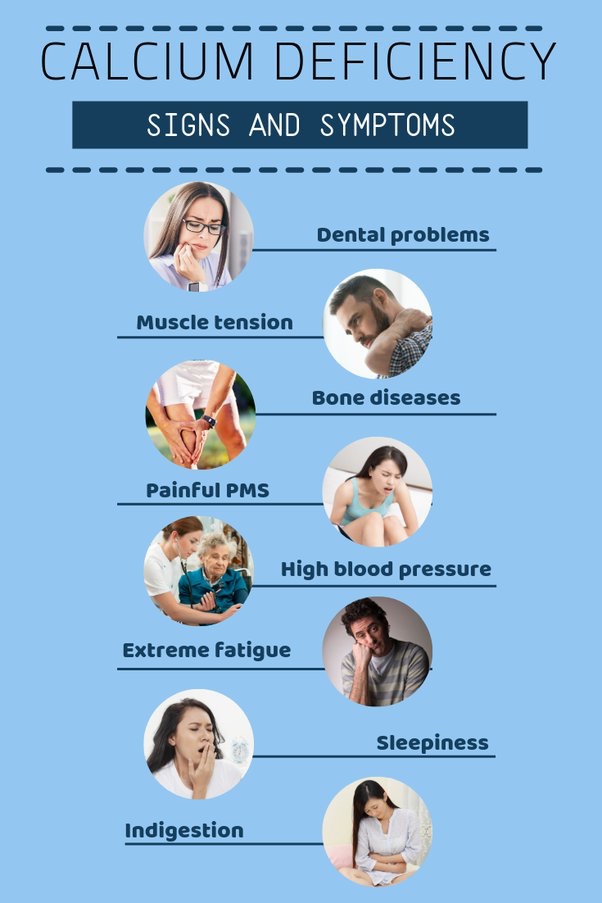
Studies reveal people with fibromyalgia often have a calcium deficiency. Calcium is the main content in bones and joints and is important in muscle contraction. Low calcium can cause muscle cramps, fatigue, lack of energy and can also lead to insomnia. In fibromyalgia our muscles remain tight and have a difficult time relaxing and contracting. Adding a calcium deficiency on top of fibromyalgia can possibly heighten the tight muscles and other symptoms. Here is a short article about fibromyalgia and calcium deficiency.
You can read more about calcium deficiency here.
Magnesium
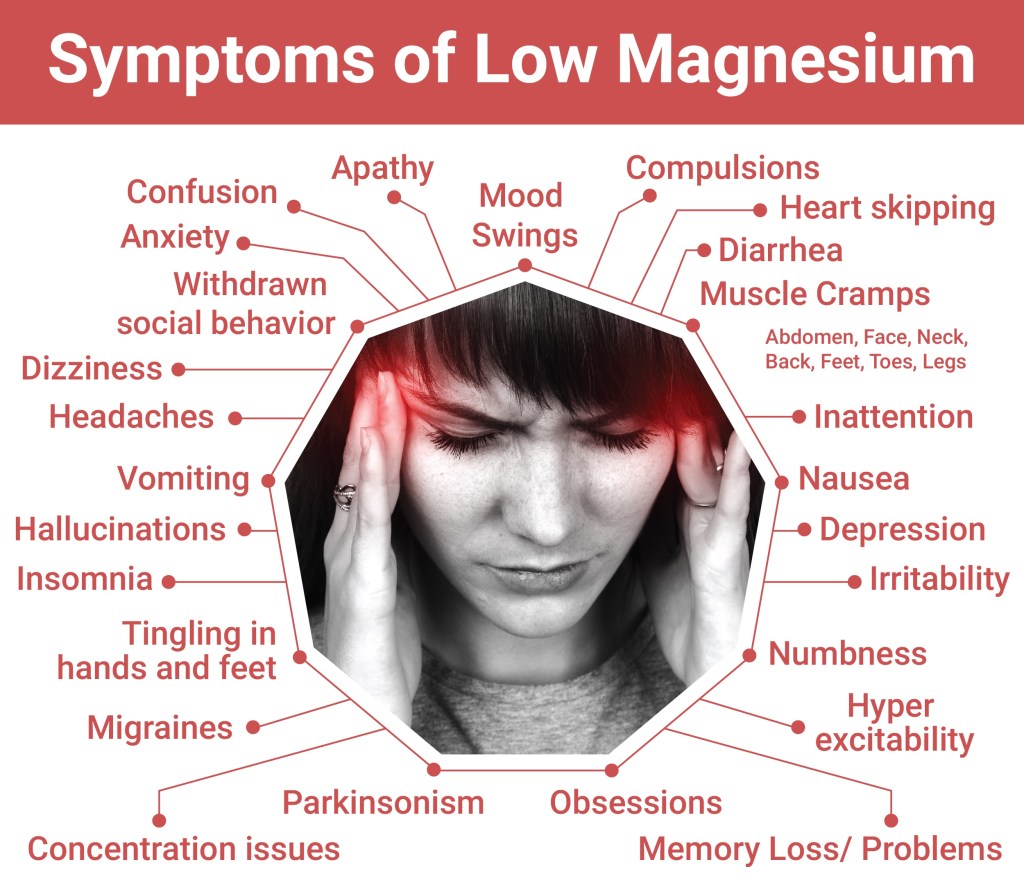
Magnesium plays a crucial role in our bodies – muscle and nerve functioning and energy production. Magnesium deficiency is associated with muscle cramps, fatigue, sleep disturbances, and anxiety. Again the result of a magnesium deficiency are all the common symptoms of fibromyalgia. Women with fibromyalgia are often seen to exhibit lower magnesium levels. Magnesium supplements are often recommended to help relieve fibromyalgia pain and other symptoms. Ever hear of Epsom salt?! You can purchase it at a pharmacy. Magnesium is the main ingredient in it. We are often told to soak in a tub with Epsom salt to help relax muscles. It is said that Epsom salt will be absorbed through our skin as we soak in the bath. However, this theory has not been proven. For myself Epsom salt makes me feel nauseous after. Doctors always told me it was because my body absorbs too much magnesium. You can read more about Epsom salt here.
You can read more about magnesium deficiency here.
Vitamin d
Vitamin d deficiency is frequently seen in people with fibromyalgia. It is common to have lower vitamin d levels during the winter months. We produce vitamin d when sunlight hits our skin. There are many symptoms of vitamin d deficiency. Some symptoms include muscle cramps/soreness body aches, fatigue/weakness,exhaustion and decreased endurance – which overlap with fibromyalgia symptoms. A study revealed people with fibromyalgia who used vitamin d supplements reported reduced musculoskeletal pain and helped improve their quality of life. You can read more about the study here.

You can read more about vitamin d deficiency here.
One can try to up their iron, magnesium, calcium and vitamin d thorough your diet to try to raise the levels. For myself, I have decided to add in supplements as it can be rather time consuming to keep track of it through diet alone. You can discuss with your doctor how many mgs of each supplement you may need to take. The supplements can be found in many different dosages. You can even consult a pharmacist to help guide you.