Fibromyalgia can be a very confusing condition. Not all healthcare providers believe fibromyalgia derives from the same body system issues. Some classify fibromyalgia as arthritis, others state it is neurological and then there are still health care providers out there that believe fibromyalgia is a mental illness. The one question we all ask is “Does fibromyalgia initiate an inflammatory response in the body? If one was to do a quick google search the results quickly reveal fibromyalgia does not produce inflammation in the body. However, many of the current speakers at fibromyalgia summits (usually doctors) state there is actually inflammation – neuro inflammation. The regular blood test to check for over all body inflammation does not seem to diagnose this inflammation. This makes it difficult to measure the actual inflammation seen in the body with fibromyalgia!
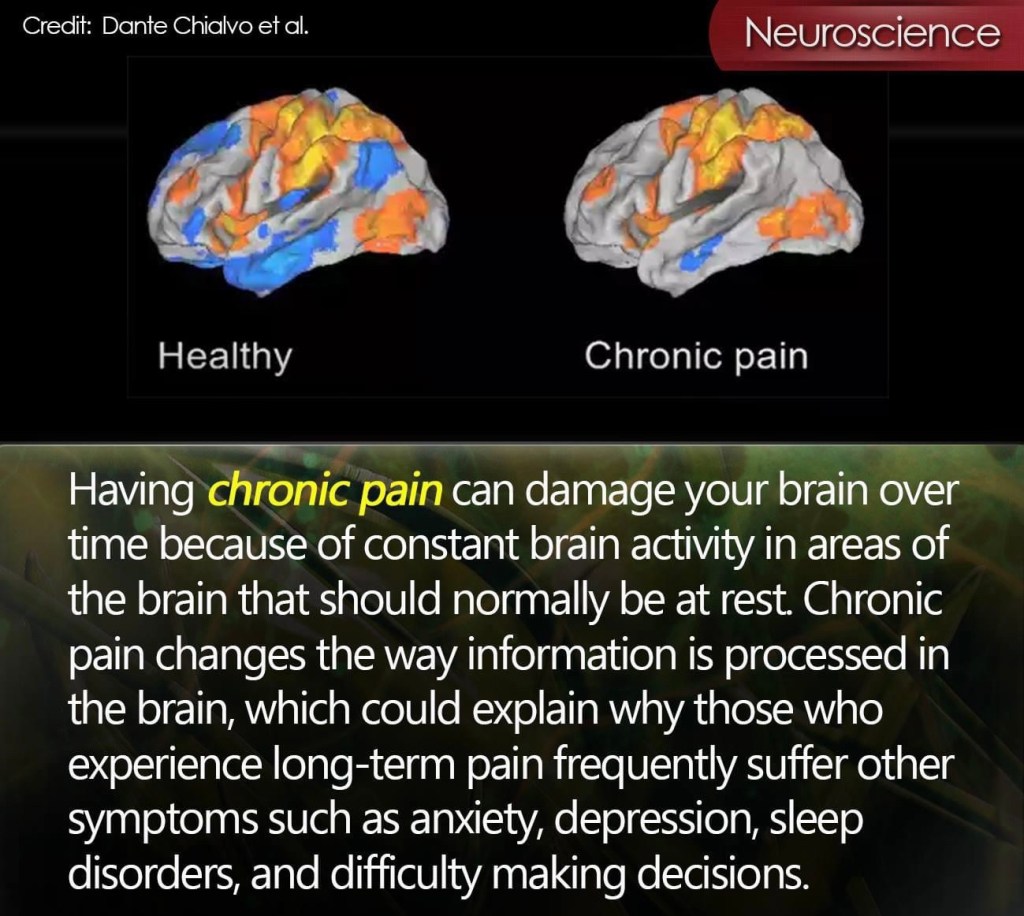
A 2018 study revealed that there appears to be increased neurological derived inflammatory mechanisms taking place in the peripheral tissues , spinal cord and brain in people with fibromyalgia! Why do doctors not know about these studies on neuroinflammation? Is it because these were just smaller studies and more evidence is needed? Regardless, these results were logged at the end of this study.
The study suggests that neuropeptides, chemokines and cytokines are all affected and cause activation of the innate and adaptive immune systems. I had no idea what these two systems were so I had to do further research. The innate immune system is the bodies first line of defense against invading pathogens while the adaptive immune system is set out to destroy the invading pathogens. As this process takes place, several peripheral clinical features of fibromyalgia are produced – swelling and dysesthesia ( unpleasant feelings in the body). The central nervous system may also be influenced thus causing changes in cognition and produces fatigue. As a result, stress related psychological mechanisms and emotional stress is triggered. All this will increase neuro inflammation. Food for thought ( my own opinion) is this why fibromyalgia is known to cause flu like symptoms in many people with fibromyalgia? I often have daily flu like symptoms and when I get sick the illness seems to last even longer compared to those I know without fibromyalgia. Is it the innate and adaptive immune system causing these symptoms? If both the innate and adaptive immune system are at play – is this more evidence that fibromyalgia may have an autoimmune component? I don’t have these answers for you all, but when I read this study, this are the questions that kept floating through my mind. Maybe one day this study will give us more insight into fibromyalgia.
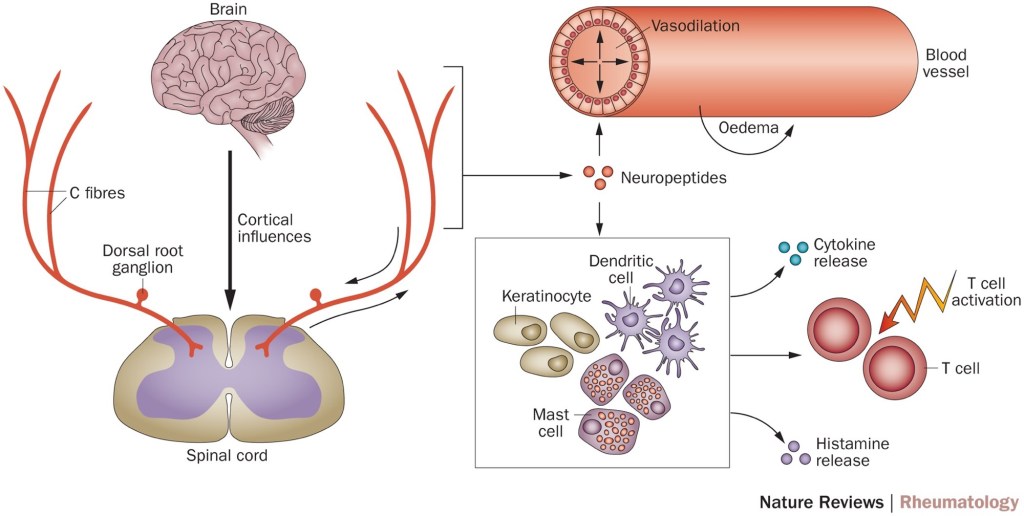
When you put all this information together, it does make sense. We are always told that these are all fibromyalgia symptoms, but no one ever explains why. This study breaks it down. Hopefully the explanation I gave wasn’t too scientific. Here is the link for the 2018 study. It is only the summary – the study in its entirety doesn’t seem to be available anywhere.
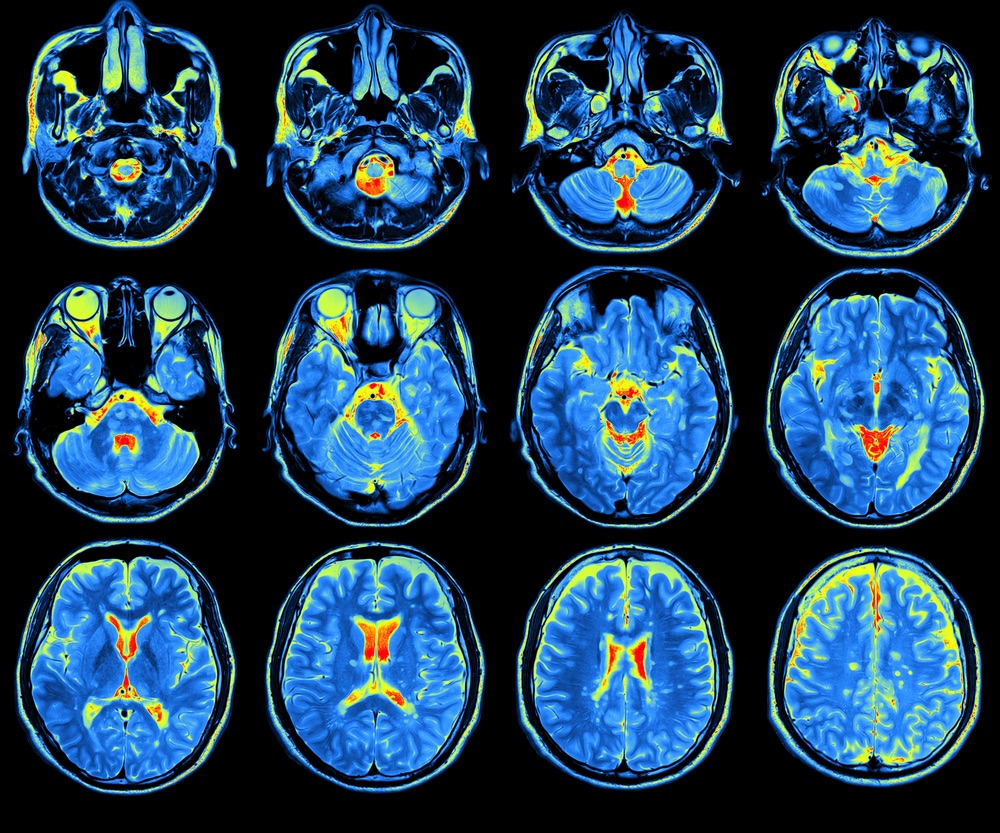
Another study done in 2021 on neuro inflammation using PET scans. There is not much for me to summarize as this study does not give much details. I will include the link. Again the results revealed that people with fibromyalgia showed a significant higher neuroinflammation than those in the control group. Conclusion – abnormal neuroinflammation can be an important pathological factor in fibromyalgia. The study revealed critical regions affected by neuroinflammation – which could help improve diagnosis and effective medical treatment for fibromyalgia.
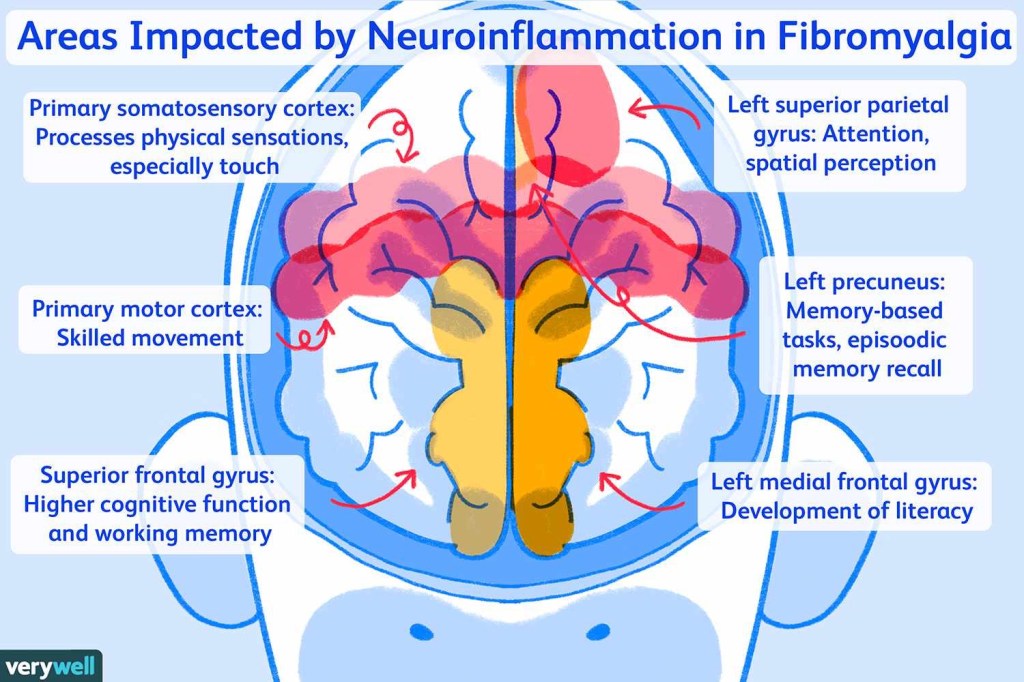
A third study completed in 2022, using Diffusion kurtosis imaging was also completed. By using this technique, microstructural alterations associated with neuroinflammation were able to be observed. Again, the results showed that people with fibromyalgia have significantly higher neuro inflammation then thee control group. The report stated that the results will help provide valuable information in regards to brain neuroinflammation. To read the study visit here.

Hopefully in the near future, these studies help improve the way fibromyalgia is diagnosed and treated. There appears to be consistent results and findings at the end of all three studies – neuro inflammation is known to be prevalent in people with fibromyalgia!