I have been reading the book, ” The Invisible Kingdom”, written by Meghan O’Rourke. The chapter on doctor-patient relationship really resonated with me. I grew up in a smaller town, were your family doctor had the time to spend an adequate amount of time with you during appointments. It wasn’t out of the ordinary to ask how life was going and have a short personal conversation about family. Today, with such a shortage of doctors (in many areas of the world), finding a family doctor is near impossible. We are left attending walk in clinics, where you end up seeing a different doctor every time. Doctors and patients are not even given enough time in appointments to discuss medical concerns. We are often told to limit our visit to one or two health issues to discuss and only have maybe ten minutes in which to do this.

People living with chronic conditions, have a difficult time discussing one topic in an appointment yet alone two health issues. Having such limited one on one time together, I feel that the doctor- patient relationship is slowly beginning to fade away and has become a thing of the past. In “The Invisible Kingdom” the writer explains that doctors don’t seem to display much empathy towards patients anymore. I believe many of us suffering with fibromyalgia have been in many situations where empathy has failed to be shown. However, research states that doctors should take the time to empathize with each patient. Showing empathy often results better.

Have you ever watched the movie “Patch Adams” with Robin Williams?! It is actually based on a true story. If you have never watched it, I recommend it! “Patch” admits himself into a mental institution for suicidal thoughts at the beginning of the movie. After witnessing how doctors treat the other patients and himself while in their care, he quickly discharges himself from their care and sets out on a mission attending medical school. He graduated becoming a doctor. His goal was to help other people – taking into consideration the PERSON not just the illness. He wanted to connect with each and every patient he encountered. Patch was set out to bring joy to all patients – no matter how grim of a diagnosis they had just been given. He gained patients trust and made a huge difference in many peoples lives.
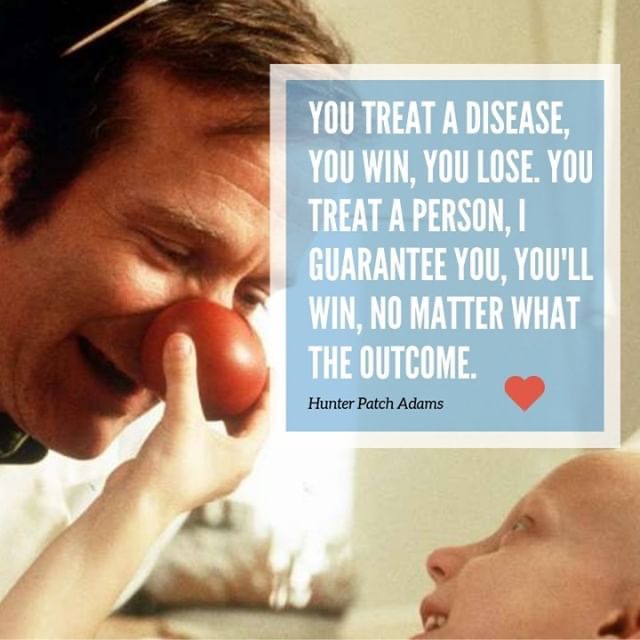
Empathy and compassion in a doctor-patient relationship can make a huge difference. Both qualities are said to be highly effective and powerful. Empathy requires health care providers to put themselves in the patient’s shoes. If the physician takes the time to pay attention to a patient’s emotions a caring treatment plan can be created. A well thought out ,treatment plan will have positive results instead of negative.

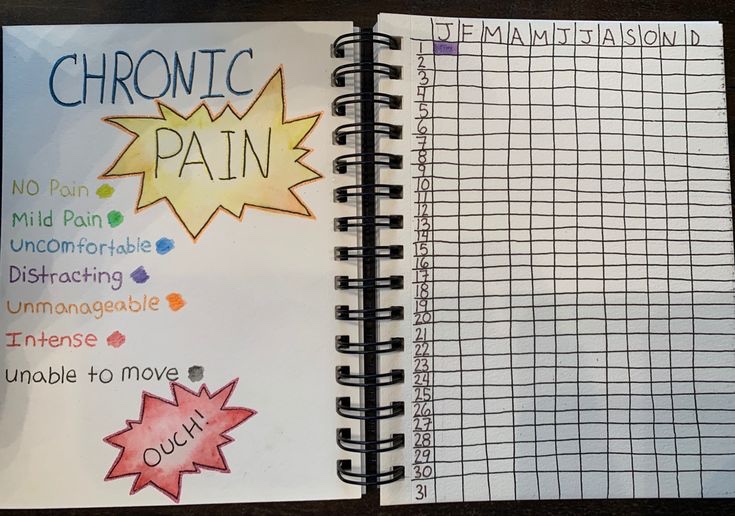
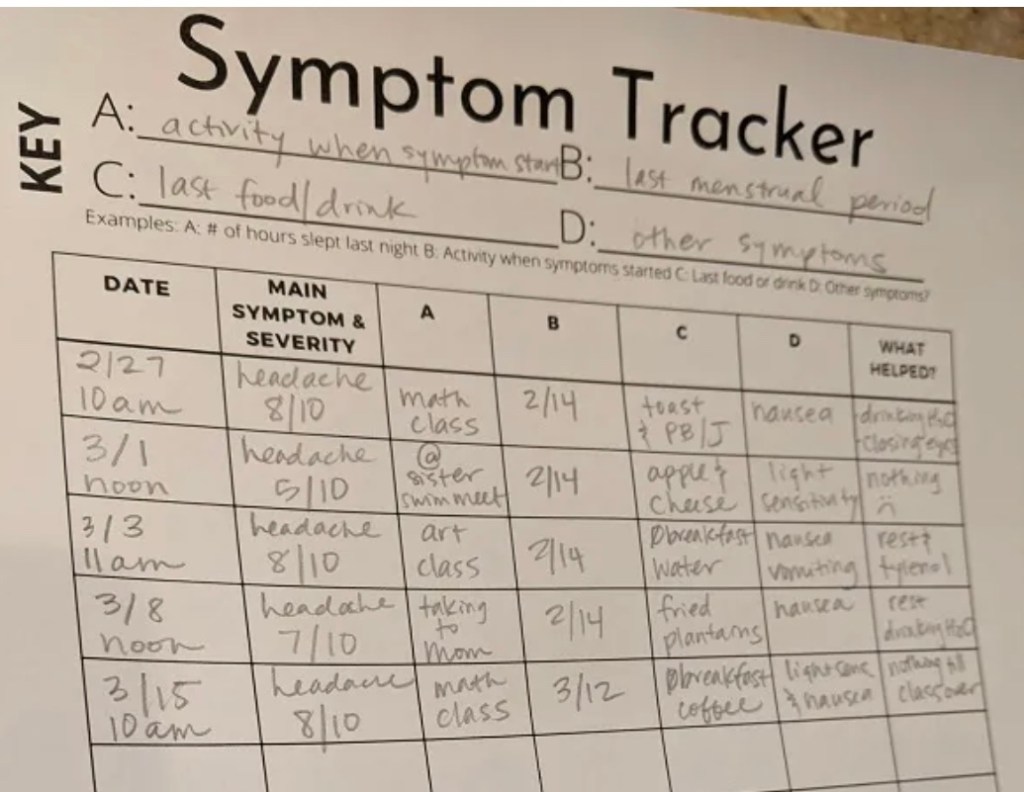
In one study, 2898 patients took part who suffered from moderate to severe chronic pain. The same doctor visited each patient at baseline, 1, and three months – having each patient fill out questionnaires. At the end of the study it was reported that chronic pain significantly decreased. It is said that by showing empathy patients are more likely to adhere to treatments and more improvements are seen. This study did not state if people with fibromyalgia were part of the study, but regardless it revealed how powerful empathy can be. You can read the results of this study here.

Empathy not only allows the doctor and patient to connect on a better level, it also is proven to lower a patient’s anxiety levels. In fibromyalgia, stress and anxiety are one culprit of raised pain levels and other symptoms. I’ll use the pain clinic I attended for an example. The clinic began to have a very negative effect on my health. I was beginning to have anxiety attacks the day prior to my appointments – which then led to a full blown fibromyalgia flare up the following morning. I never saw eye to eye with a few of the pain clinic staffing who were directly involved in my care. When I stated I felt my fibromyalgia may have been triggered by a knee injury I got the spring prior, I was told an injury was not a possible cause of fibromyalgia. An injury is considered trauma – trauma is a possible cause of fibromyalgia is it not? As the months went on staff began belittling me and told me I was making their job too difficult. I complied with treatment, but when I expressed my frustration to the mental health counsellor that all strategies were only increasing my pain – I got told I was being too negative and that mental health would not continue to see me. I always thought psychologists and counsellors were there to help a person through the tough times and help change the negative to more positive thinking. “Making their job too difficult “- in my eyes this meant they didn’t know what else to do to help me – so they put the blame on me. It is easier to blame the patient then admit the program failed to help me. I often wonder if empathy was used, if I would have had a better outcome? I soon realized I was just a number to push through their pain clinic program so it would free up a spot for their long wait list. They eventually discharged me without even speaking to me first.

Here is a video I found that brings a powerful meaning on empathy. It has been viewed 6.9 million times.